Overview of Irinotecan and Topotecan: The Topoisomerase I Inhibitors
For DNA replication and cellular division to occur, topoisomerase I is required. It is an enzyme that creates and helps repair strands of DNA. In cancer cells, it has been shown that there is an increased activity of topoisomerases. This is why topoisomerase inhibitor medications have been used in many cancer therapies. Mainly topoisomerase I is responsible for relaxing supercoiled double strands of DNA, which then allows for replication to occur. The most common topoisomerase I inhibitor medications are irinotecan and topotecan.
In 1996, irinotecan and topotecan were approved for use in the United States. Camptothecin is another topoisomerase I inhibitor, and irinotecan and topotecan were originally derived from it. Camptothecin was isolated from the Camptotheca acuminata, which is a Chinese tree. Since its discovery and use, there have been fewer toxic analogues made.
Depending on the drug, indications can vary. Commonly, they are used in advanced colorectal, ovarian, and small-cell lung cancer. There are multiple regimens, and dose administration is dependent on the specific regimen cycle it is being used for. Irinotecan has been used with other therapies, such as 5-fluorouracil (5-FU) and leucovorin (LV). Hepatic adjustments may be seen with irinotecan because it is metabolized by the liver. Compared to topotecan, it is renally eliminated, which may result in possible renal adjustments in patients. Moreover, dosage and administration can sometimes vary based on the regimen, body weight, and other patient-specific factors.
What are the differences and similarities between liposomal irinotecan and irinotecan?
- Liposomal form of irinotecan has a lipid bilayer
- SN-38 is an active metabolite of both medications
- The lipid bilayer prolongs irinotecan half-life, and it prevents it from converting to its active metabolite quicker
- The liposomal form is used for treatment in patients with metastatic adenocarcinoma of the pancreas
- These are not interchangeable medications
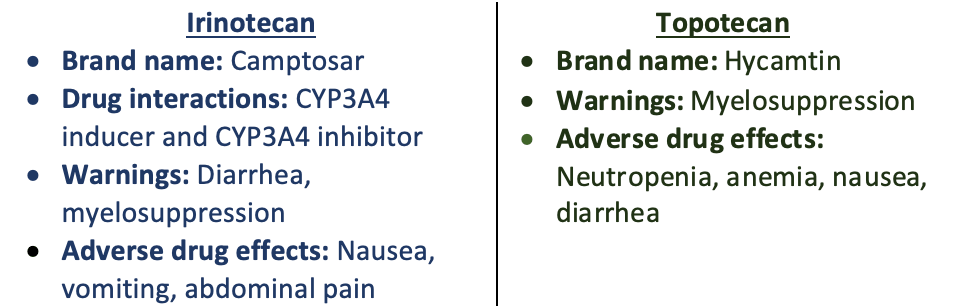
There are many chemotherapeutic medications that have extensive side effect profiles or adverse reactions associated with them. It is important to distinguish that there are acute and delayed adverse reactions. To overcome these acute and delayed adverse reactions, patients are pre-medicated. For example, the most notable toxicity seen with irinotecan is diarrhea, which is usually delayed. To overcome this, some patients will receive loperamide. Another example associated with irinotecan is its acute cholinergic syndrome, which can be treated with atropine. Overall, not all patients will be pre-medicated with the same regimens because there are patient-specific factors to account for prior to selecting treatments that mitigate and prevent adverse effects seen with these chemotherapeutic medications. The noticeable toxicities in topoisomerase I inhibitors are typically hematologic and gastrointestinal.
Irinotecan and topotecan have been used for a long time. It is important to notice that even though these medications are in the same drug class, they are not interchangeable. These medications are utilized for many different cancer types, such as advanced colorectal, ovarian, and small-cell lung cancer. Overall, staying up to date with new findings and the most current literature is important to ensure that patients receive the best-individualized therapy.
Dagmara Zajac
RxPharmacist Team
References:
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Topoisomerase Inhibitors. [Updated 2020 Sep 12]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548372/
- Topoisomerase inhibitor. Topoisomerase Inhibitor – an overview | ScienceDirect Topics. https://www.sciencedirect.com/topics/neuroscience/topoisomerase-inhibitor#:~:text=Topoisomerase%20I%20inhibitors%20include%20irinotecan,etoposide%2C%20doxorubicin%2C%20and%20epirubicin. Accessed December 13, 2022.
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Irinotecan. [Updated 2018 Apr 27]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548037/
- CAMPTOSAR®Dosage and Administration (irinotecan hcl). CAMPTOSAR® Dosage and Administration (irinotecan HCl) | Pfizer Medical Information – US. https://www.pfizermedicalinformation.com/en-us/camptosar/dosage-admin. Accessed December 13, 2022.
- Baker DE, Levien TL. Irinotecan Liposome Injection. Hosp Pharm. 2017;52(2):144-150. doi:10.1310/hpj5202-144
- HYCAMTIN® (topotecan) for injection, for intravenous use. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/020671s023lbl.pdf. Accessed December 13, 2022.
Overview of Irinotecan and Topotecan: The Topoisomerase I Inhibitors Read More »