Renal Disorders: Why Dialysis Can Help Your Kidneys “Let It Go”
Kidneys are a good example of the saying, “you don’t know what you’ve got ‘till it’s gone”. This is primarily because most people genuinely do not know they have reached an irreversible loss of kidney function until it is too late. You may be wondering how such a drastic decline in kidney function can silently progress under the radar. To answer why and how renal dysfunction typically goes undetected, it is important to first understand what makes the kidneys unique to other aspects of the body.
Your vital organs are all special with their own unique abilities and superpowers. For example, the liver is the only organ in your body with the capacity to regenerate itself. The key quality to remember when it comes to kidneys is they like to both work together as a team. Working together may not seem as much of a superpower, but it is incredibly useful when one kidney compensates for the impaired function of the other kidney. Even alone, a single kidney’s working nephrons can also compensate for the loss or degeneration of other nephrons within the organ itself.4 The kidneys are so highly adaptable they do a stellar job of making a sinking ship look like it is sailing, but this also means trying to identify declining renal function early to prevent progression of disease can be very challenging. Many patients will find themselves in this position and although we can screen for risk factors, a decline in renal function will likely remain silent and unrecoverable.
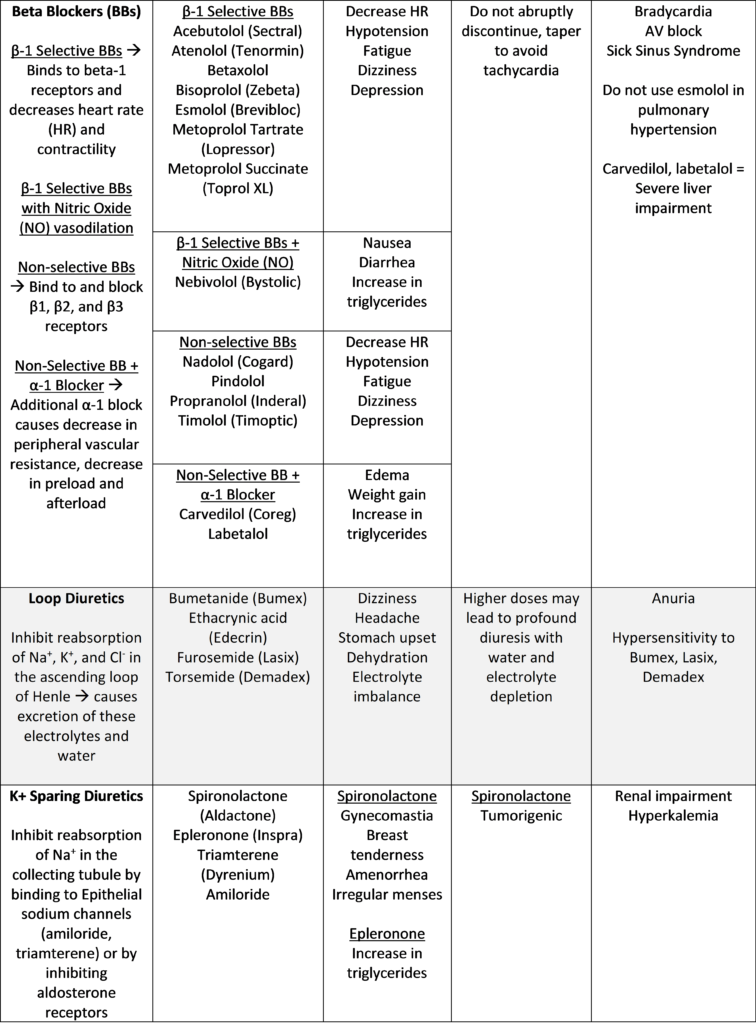
Outlined above are the differences between acute kidney injury (AKI) and chronic kidney disease (CKD). Since kidney damage is irreversible, prevention of AKI and CKD is paramount. For renal disorders, there is no real cure as therapy is typically supportive and dependent on the etiology.1 With this in mind, you may be wondering how we can go about being more proactive towards kidney disease. Clinical surveillance is an example of an effort that serves this very cause. If we take a look at the Nephrotoxic Injury Negated by Just-in-time Action (NINJA) project, we can see a 38% decrease in AKI exposure (estimated 633 cases avoided) and a 64% decrease in AKI (398 cases avoided) due to surveillance providing a timelier approach in identifying AKI.2
Although we have medications in place to treat the secondary complications and further progression of CKD, patients who do progress to end stage renal disease will find themselves dependent on dialysis in the absence of a kidney transplant.1 So, what happens to patients who officially progress to end stage renal disease and require dialysis? Well, the good news is there are some options. Patients can decide between hemodialysis (HD) or peritoneal dialysis (PD).1 HD requires several visits a week to a HD center and may cause further decline in residual renal function as compared to PD, which may be conveniently performed at home but has a higher risk of peritonitis.1
The title of this post references Frozen because that’s exactly how dialysis works: by letting all the toxins in your body go. When your kidneys are damaged, they cannot filter out all the toxins in your body as well so waste products and fluid can accumulate to a fatal degree.3 Dialysis helps prevent this accumulation by allowing toxins to essentially move from the blood to the dialysate, thereby filtering the blood and acting in place of the kidneys.1
References
- DiPiro, Joseph T. Pharmacotherapy: A Pathophysiologic Approach. New York: McGraw-Hill Medical, 2020. Print.
- Goldstein SL, Mottes T, Simpson K, et al. A sustained quality improvement program reduces nephrotoxic medication-associated acute kidney injury. Kidney Int. 2016;90(1):212-221. doi:10.1016/j.kint.2016.03.031.
- Dialysis. NHS. Accessed January 25, 2021. https://www.nhs.uk/conditions/dialysis/.
- Fattah H, Layton A, Vallon V. How Do Kidneys Adapt to a Deficit or Loss in Nephron Number?. Physiology (Bethesda). 2019;34(3):189-197. doi:10.1152/physiol.00052.2018.
- Bynum W. When kidneys fail. Lancet. 2014;383(9931):1798-1799.
Renal Disorders: Why Dialysis Can Help Your Kidneys “Let It Go” Read More »