As per the Centers for Disease Control and Prevention (CDC), 34.2 million people, or 1 in every 10, in the United States have diabetes. Diabetes is 7th on the list of leading causes of death while the total estimated medical costs and costs associated with lost work and wages equates to an estimated $327 billion.
Diabetes, otherwise known as increased sugar levels (hyperglycemia) may be a result of decreased insulin secretion, decreased insulin sensitivity, or both. It can present itself in one of two forms of the following:
- Type 1
- Autoimmune destruction of beta cells
- Loss of insulin production
- Must use insulin injections
- Type 2
- Insulin resistance
- Decreased insulin production over time
- Associated with obesity, physical inactivity, family history
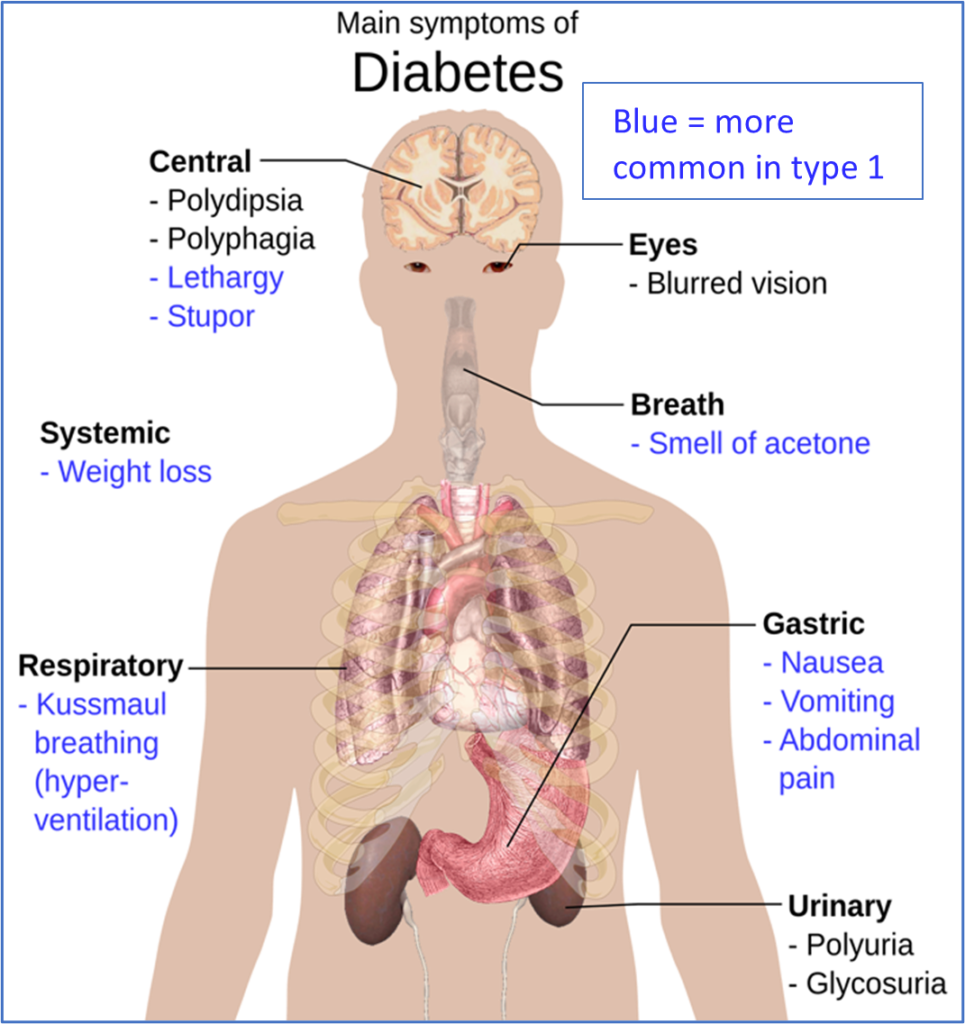
- Signs and symptoms of diabetes include:
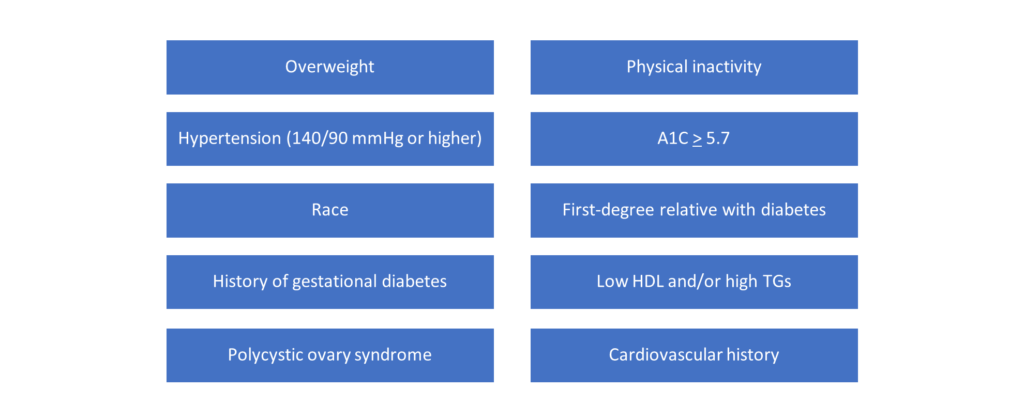
- Risk factors:
- General Screening Criteria:
- All patients with BMI greater than or equal to 25 kg/m2 + 1 risk factor
- Children/adolescents with obesity + 1 risk factor
- 45 years old if no risk factors are present
- Pregnant women at 24-48 weeks
- Diagnosis (per ADA guidelines):
| Prediabetes | Diabetes |
| ->Fasting plasma glucose (FPG) 100-125 mg/dL; or ->2-hour glucose after glucose tolerance test 140-199 mg/dL; or ->A1c 5.7-6.4% | ->Symptoms + random plasma glucose > 200 mg/dL; or ->2-hour glucose after glucose tolerance test > 200 mg/dL; or ->FPG > 126 mg/dL; or ->A1c > 6.5% |
- Glycemic targets (per ADA guidelines):
- A1c < 7%
- 80-130 mg/dL pre-prandial plasma glucose
- < 180 mg/dL post-prandial plasma glucose
- A1c should be measured quarterly if not at goal
- Or twice yearly if at goal
- (A1c – 2) x 30 = average blood glucose
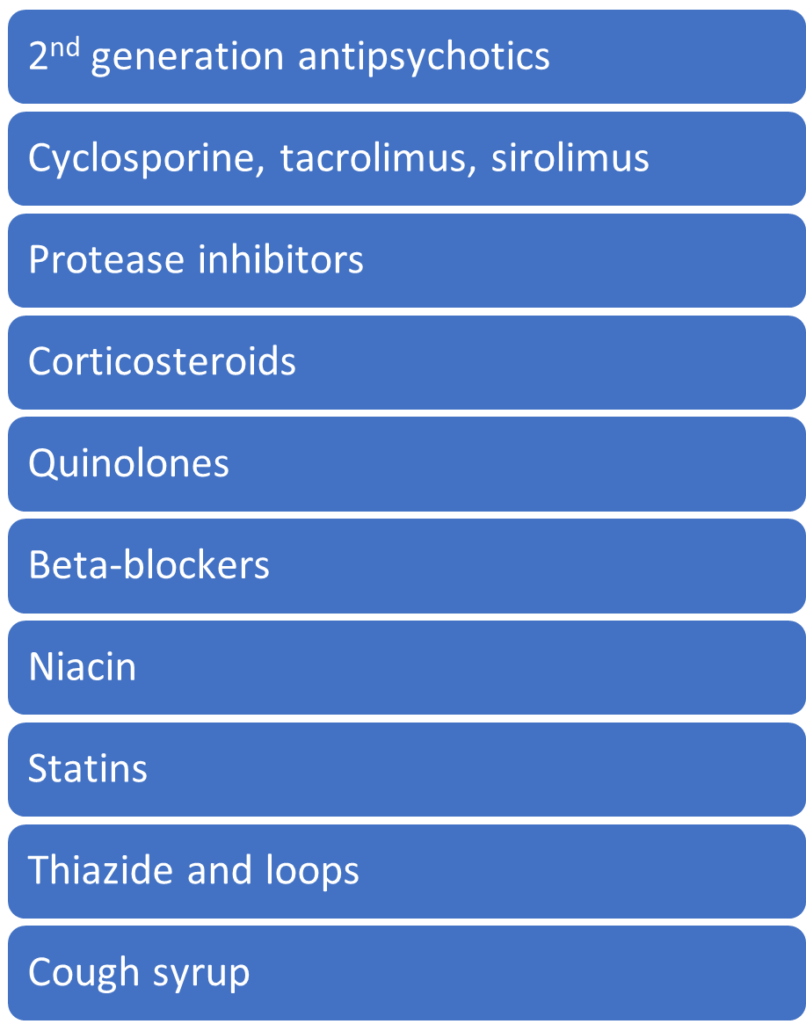
- Drugs that may increase blood glucose levels:
- Non-drug treatment options:
- Smoking cessation
- Weight loss
- 3500 kcal weekly reduction = 1 lb weight loss
- Waist circumference < 35 inches for females and < 40 inches for males
- Nutrition
- Carbs from vegetables, fruits, grains, and dairy
- Omega-3 fatty acids and fiber
- Limit saturated fat, cholesterol, and sodium
- 15 g = 1 serving of carbohydrates
- Physical activity
- 150 min/week, moderate intensity
- No more than 2 consecutive days off
- Resistance training at least 2x/week
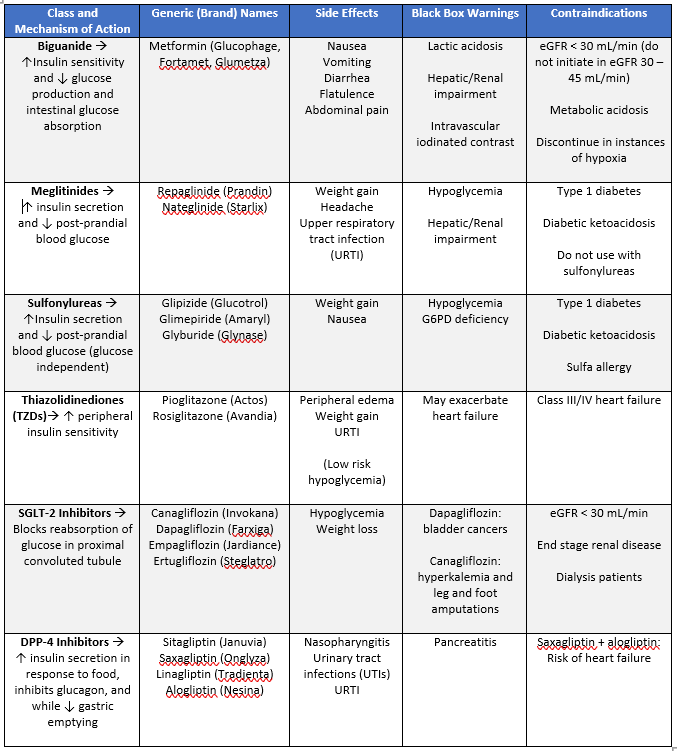
- Additional notes on oral drug classes:
- Biguanides
- Take with food
- Use of alcohol increases the risk of lactic acidosis
- Discontinue before any imaging with iodinated contrast; resume after 48 hrs
- Meglitinides
- Take 1-30 minutes before meals
- If skipping a meal, skip dose as well
- Sulfonylureas
- Take with breakfast
- Exception: Glipizide IR 30 minutes before breakfast
- Glyburide – avoid in elderly and patients with renal impairment
- Take with breakfast
- Thiazolidinediones
- Take with meals
- May take weeks to take effect
- Additional warnings:
- Bladder cancer (pioglitazone only)
- Risk of macular edema
- Fracture risk
- Hepatic failure
- Resumption of ovulation
- SGLT-2 Inhibitors
- Caution when taking with diuretics and NSAIDs (due to risk of hypotension and acute kidney injury)
- Additional warnings:
- Genital infections
- Hypotension
- Increased LDL
- Renal insufficiency
- Ketoacidosis
- Monitor K+ with Canagliflozin
- DPP-4 Inhibitors
- Take in the morning
- Biguanides
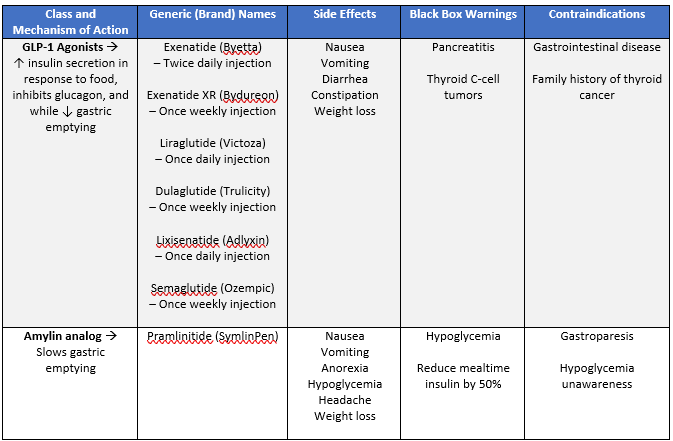
Additional notes on injectable drug classes:
- GLP-1 Agonists:
- Exenatide and lixisenatide are administered 60 minutes before a meal
- All others given without regard to food
- Amylin Analog
- Used in treatment of both type I and II diabetes
- Reduce mealtime insulin by 50%
- Drug treatments (Insulin)
- For all insulins:
- Side effects: weight gain
- Warnings; hypoglycemia, hypokalemia
- Never use pens for more than one individual
- Most are 100 units/mL concentration
- High risk medications
- Dosing strategies
- Basal insulin
- Long or intermediate acting
- Mainly affect fasting blood glucose
- Bolus insulin
- Rapid or short acting
- Two purposes:
- Prandial (mealtime) & correction (acute elevation)
- Basal insulin
- For all insulins:
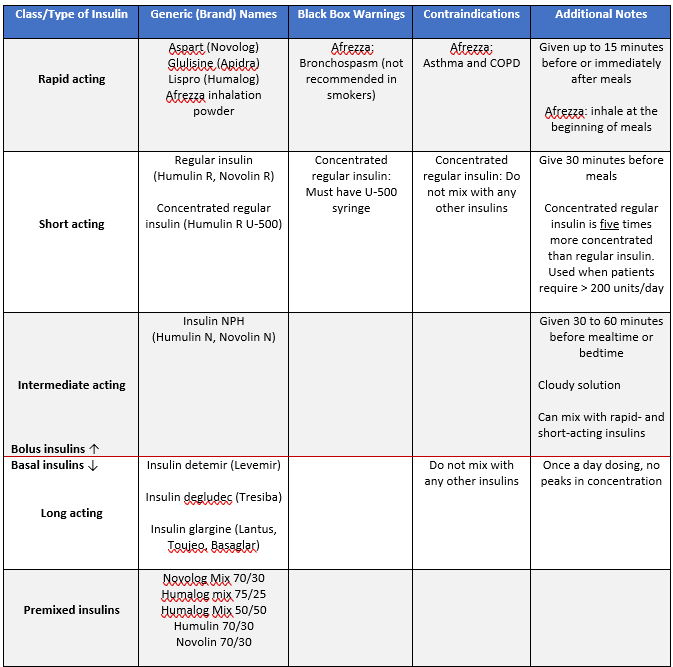
- Insulins that do not require a prescription:
- Regular insulin, NPH, and the premixed 70/30 combination
- Insulin dosing for Type I diabetes:
- Rapid-acting and basal insulin preferred
- If using NPH and regular insulin
- 2/3 NPH, 1/3 regular
- Initiating basal/bolus insulin:
- Calculate total daily dose (TDD)
- 0.6 units/kg/day using TBW
- Step 2: Divide TDD
- 50% basal
- 50% bolus
- Step 3: Divide the bolus among 3 meals
- Calculate total daily dose (TDD)
- Based on the amount of carbohydrates in a meal, meal-time insulin can be adjusted using rule of 500 (rapid-acting insulin) or rule of 450 (regular insulin)
- (500 or 450)/TDD = g of carbs covered by 1 unit of insulin
- Correction factor/dose
- Factor:
- Determines how much blood sugar will drop for every 1 unit of insulin. Uses the rule of 1800 (rapid-acting insulin) or rule of 1500 (regular insulin)
- (1800 or 1500)/TDD = correction factor for 1 unit of insulin
- Determines how much blood sugar will drop for every 1 unit of insulin. Uses the rule of 1800 (rapid-acting insulin) or rule of 1500 (regular insulin)
- Factor:
- Dose:
- Amount of insulin required to bring blood glucose back to normal: [(blood glucose now) – (target blood glucose)]/ correction factor = correction dose
- General treatment algorithm for Type II Diabetes:
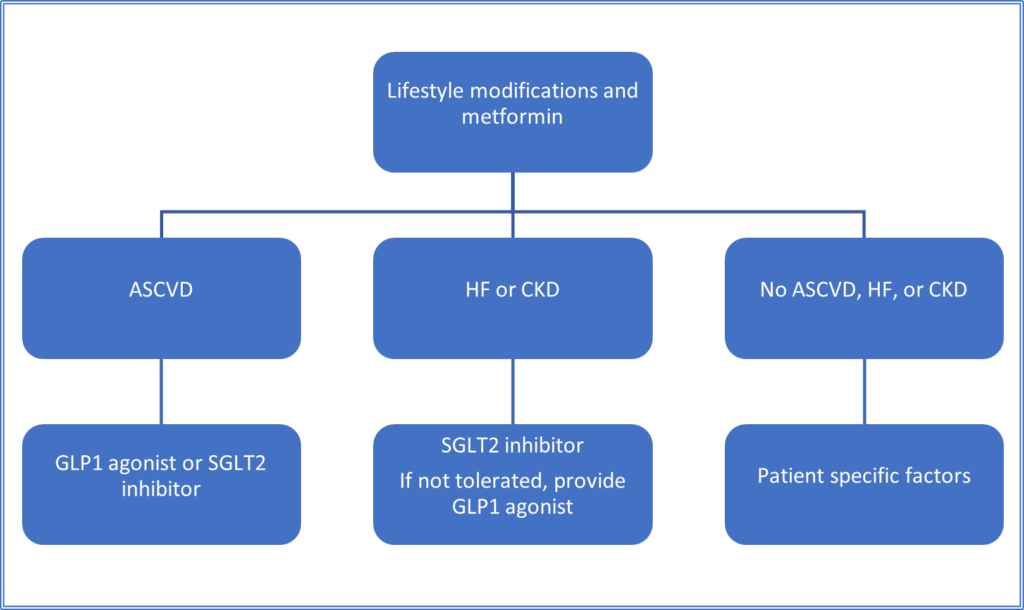
- For A1c greater than or equal to 8.5%: Jump straight to dual treatment
- A1C > 10%: Think insulin
- Cardiovascular benefit:
- GLP1 agonists: liraglutide, semaglutide, exenatide
- SGLT2 inhibitors: empagliflozin, canagliflozin
- Patient-specific factors
- Drugs that minimize hypoglycemia:
- DPP4 inhibitor, GLP1 agonist, SGLT2 or TZD
- Drugs that promote weight loss:
- GLP1 agonist or SGLT2 inhibitors
- Drugs with cost concerns:
- Sulfonylurea or TZD
- Drugs that minimize hypoglycemia:
- Combinations to avoid:
- DPP4 inhibitors + GLP1
- Sulfonylureas + insulin
- Insulin dosing for Type II diabetes:
- Initiate basal insulin after patient fails to reach or maintain goal on multiple oral therapies
- Starting dose: 0.1-0.2 units/kg/day or 10 units/day
- Titrate by 10-15% or 2-4 units once or twice weekly until fasting blood glucose at goal
- If patient reaches fasting blood glucose goal but their A1c is still above goal:
- Consider the addition of rapid acting mealtime insulin or GLP-1 agonist
- Insulin administration:
- Abdomen is the injection site (avoid belly button)
- May also inject in thighs, buttocks, arms
- Be consistent with administrations
- Prime before each dose
- Rotate sites
- Hypoglycemia is common with insulin products, thus important to be aware of what to look out for and how to treat it
- Defined as a blood glucose < 70 mg/dl
- Symptoms: sweating, pallor, irritable, hunger, lack of coordination, sleepy
- Beta blockers mask most except hunger and sweating
- Treatment
- Consume 15-20 g of glucose/simple carbohydrates
- Recheck glucose levels after 15 minutes
- Repeat if needed
- Eat a small meal/snack to prevent recurrence
- Glucagon is used only if patient is unconscious
- Diabetes in pregnancy
- Gestational diabetes: during pregnancy
- Risks
- Macrosomia
- Hypoglycemia at birth
- Obesity and type 2 diabetes
- Management
- Lifestyle modifications
- Insulin added if needed (preferred)
- Metformin and glyburide used
- Goals:
- Fasting < 95 mg/dL
- 1-hour post-meal less than or equal to 140
- 1-hour post-meal less than or equal to 120
- Risks
- Gestational diabetes: during pregnancy
We hope this review helped refresh your clinical knowledge on diabetes. Next up, we will take a look at dyslipidemia.
Best of luck,
Sam Tamjidi
RxPharmacist Team
References:
- National Diabetes Statistics Report, 2020. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed October 26, 2020.
- Micromedex Solutions. Greenwood Village, CO: Truven Health Analytics. http://micromedex.com/. Accessed October 26, 2020.
