Antibiotics are commonly prescribed. In 2021, there were 211.1 million oral antibiotic prescriptions given by healthcare professionals in the outpatient setting. In other terms, that is an estimated 636 oral antibiotic prescriptions per 1000 individuals. To compare this to previous year’s statistics, in 2020, there were 201.9 million oral antibiotic prescriptions given by healthcare professionals in the outpatient setting, meaning 613 oral antibiotic prescriptions per 1000 individuals. Clearly, this shows that the number of antibiotic prescriptions keeps increasing.
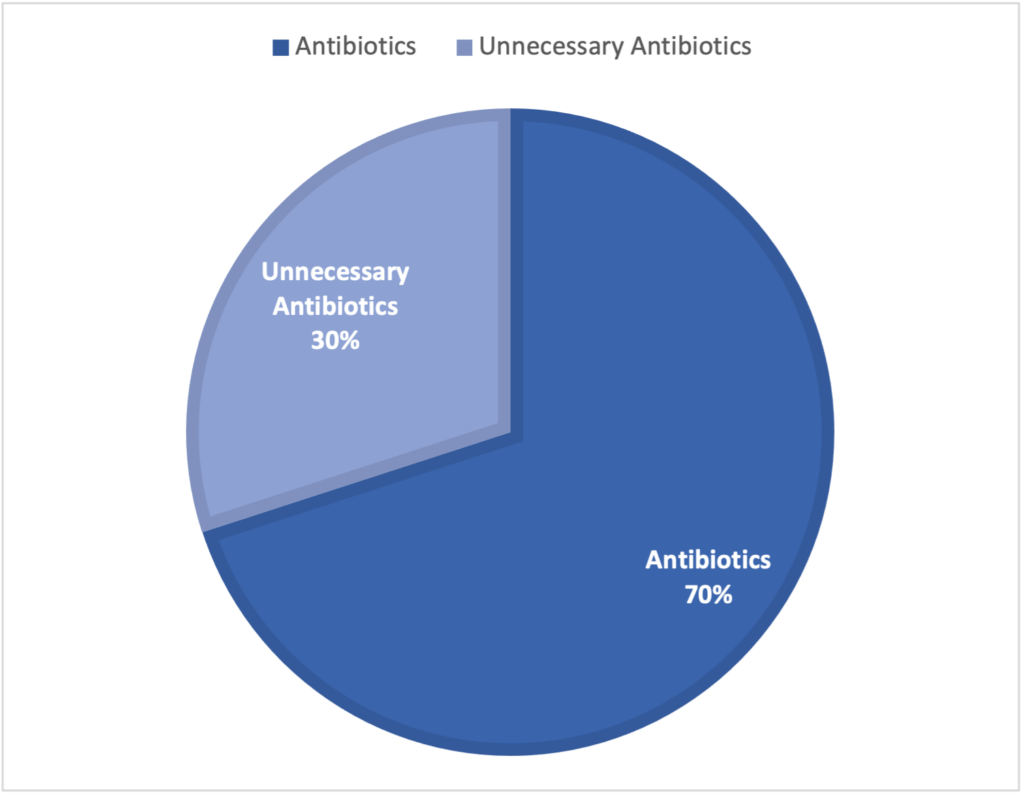
According to the Centers for Disease Control (CDC), about 30 % of antibiotics are prescribed unnecessarily in the outpatient setting (See Figure 1). With that being said, it is crucial to discuss and understand the issue of antimicrobial resistance. Due to increased unnecessary prescribing of antibiotics, antimicrobial resistance is on the rise and it has become a serious matter and threat to not just local health, but also global public health. Since the pharmaceutical industry isn’t providing new drugs on the market to make up for the increase in antibiotic resistance, then what has been done to address this growing problem? One answer to that question is antibiotic stewardship programs.
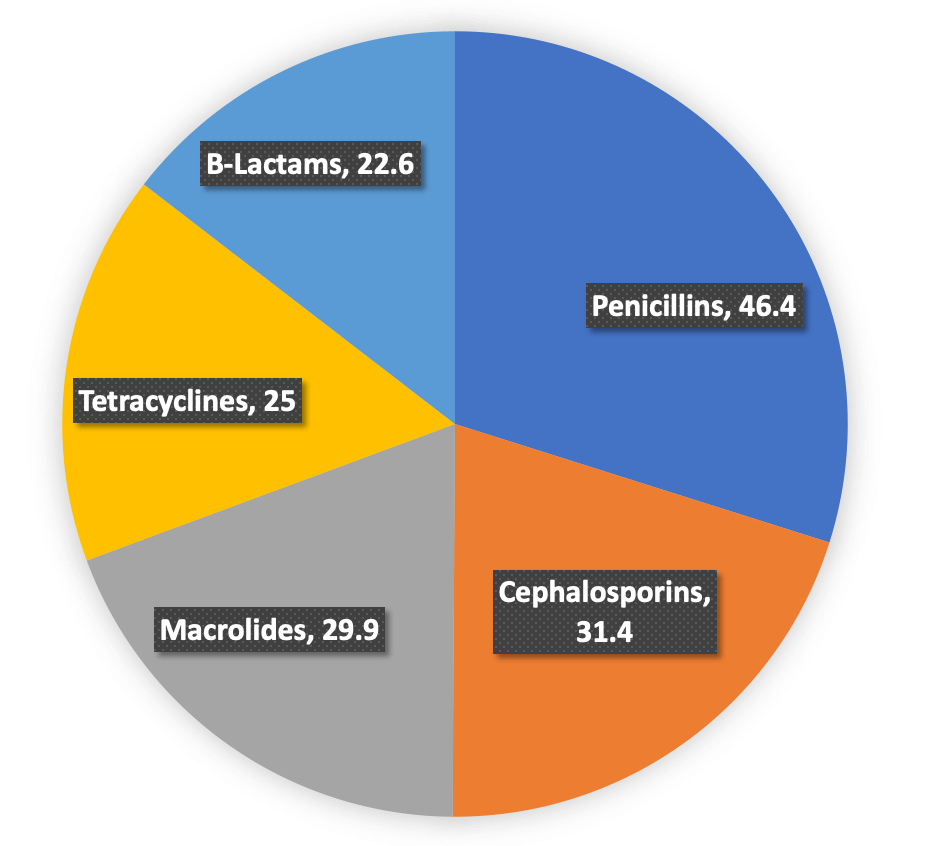
According to CDC 2021 annual report, the top 5 most common oral antibiotic classes prescribed in the United States were:
Due to antimicrobial resistance, antibiotics lose their effectiveness in fighting off infections. This has led to other implications, such as prolonged hospital stays, increased costs, treatment failures, and much more. On average, patients will be in the hospital for 13 days due to antimicrobial resistance. Therefore, multidrug resistance (MDR) has become a significant challenge in healthcare and has worsened the antimicrobial resistance issue. For example, globally, 500,000 new cases of MDR tuberculosis are diagnosed yearly. On top of everything, it has been shown that the COVID-19 pandemic has set to increase the threat of antimicrobial resistance as well. Overall, pharmaceutical companies have drifted away from this drug development area, which is why there has been a decrease in new antibiotic development for many years.
Antibiotic stewardship programs aim to help this growing problem by improving the use of antibiotics. Physicians and pharmacists have led the majority of antibiotic stewardship programs. These programs ensure that clinicians prescribe antibiotics only when it is necessary, prescribe antibiotics that cover the necessary infection, and do not expose patients to unnecessary antibiotics. To be in accordance with the Centers for Medicare and Medicaid Services, the Joint Commission made it a requirement for hospital settings to have antibiotic stewardship programs implemented. This is a huge win in reducing inappropriate antibiotic use. Antibiotic stewardship programs can be found in various settings, such as hospital settings, outpatient settings, nursing homes, and resource-limited settings. The CDC website has a page with core elements designated to each antibiotic stewardship program setting to understand that each program may differ depending on its location.
Antibiotic resistance has been on the uptrend for quite a while. It is important to know why antibiotics must be carefully prescribed. Antibiotic stewardship programs are one way that this growing problem is being addressed. Hopefully, we will see that antibiotic stewardship efforts have decreased the issue of antibiotic resistance over time.
References:
- Majumder MAA, Rahman S, Cohall D, et al. Antimicrobial Stewardship: Fighting Antimicrobial Resistance and Protecting Global Public Health. Infect Drug Resist. 2020;13:4713-4738. Published 2020 Dec 29. doi:10.2147/IDR.S290835
- Barlam TF. The state of antibiotic stewardship programs in 2021: The perspective of an experienced steward. Antimicrob Steward Healthc Epidemiol. 2021;1(1):e20. Published 2021 Aug 5. doi:10.1017/ash.2021.180
- Measuring outpatient antibiotic prescribing. Centers for Disease Control and Prevention. https://www.cdc.gov/antibiotic-use/data/outpatient-prescribing/index.html. Published October 5, 2022. Accessed December 1, 2022.
- Outpatient antibiotic prescriptions — United States, 2021. Centers for Disease Control and Prevention. https://www.cdc.gov/antibiotic-use/pdfs/Annual-Report-2021-H.pdf. Published October 7, 2021. Accessed December 1, 2022.
- Outpatient Antibiotic Prescriptions – United States, 2020. Centers for Disease Control and Prevention. https://www.cdc.gov/antibiotic-use/pdfs/Annual-Report-2020-H.pdf. Published October 7, 2021. Accessed December 1, 2022.
- Core elements of antibiotic stewardship. Centers for Disease Control and Prevention. https://www.cdc.gov/antibiotic-use/core-elements/index.html. Published April 7, 2021. Accessed December 1, 2022.
