Currently, in a rapidly evolving healthcare landscape, the world of medicine relies heavily upon facts and evidence. As a healthcare professional, making informed decisions about medications, treatments, and interventions is crucial. What role does evidence-based medicine (EBM) play into all of this? Let’s investigate.
As a pioneer in EBM, Dr. David Sackett’s most recent definition of it is: “The integration of best available evidence with clinical expertise and patient values into the decision-making process for patient care.”1 EBM serves to provide a scientific framework for being able to ask and provide answers to clinical questions while keeping in mind the needs of the patient in different clinical settings. The components of EBM fall into three categories: best available evidence, clinical expertise, and the values and preferences of the patient.
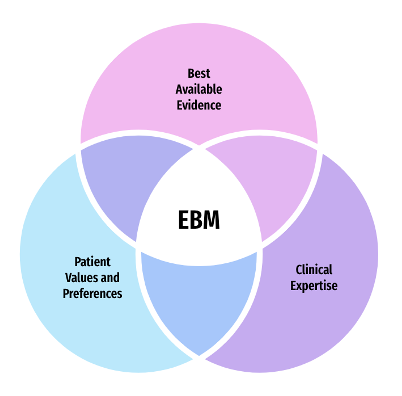
- (Best Available) Evidence: refers to the findings from clinical research, from the best available resource that is relevant to patient care.2 These findings can be from systematic reviews, and clinical research from experimental and observational studies. It is the gathering of research information to help inform decision-making.
- Clinical Expertise: involves using clinical skills and experience to evaluate evidence related to the patient’s current health status.2 Pharmacists have the skills and experience related to pharmacotherapy and clinical service. They can be valuable resources in both the access and translational aspects of pharmacotherapy evidence as this is relevant to patient care.
- Patient Values and Preferences: refer to the goals, expectations, and beliefs that patients have for decisions and their outcomes.2 The values and preferences of a patient regarding the healthcare choices they make or decide upon are based on their beliefs, attitudes, cultural, and spiritual factors. It is vital to ensure that delivery of healthcare is mindful of all these factors and that they are used as a guide when it comes to clinical decisions.
Another way to view EBM is to look at it as a course of action: you receive a question, you search for the data to help answer the question, and then you end your search by relaying the information found. This course of action, in fact, can also be outlined in the 4 steps below.2
Step 1: Ask an Appropriate and Answerable Clinical Question
○ Make sure it is properly structured and guides the evidence search
○ What is the focus of the question? What type of information are you looking for?
Step 2: Find the Evidence
○ Search published literature from relevant resources
○ PubMed or Cochrane Library
Step 3: Appraise the Evidence Found
○ Review relevant information (all evidence ≠ each other) along with internal validity
○ Per the “Hierarchy of Evidence”, systematic reviews/meta-analyses are ranked the highest, then randomized controlled trials, and then cohort studies
Step 4: Apply the Evidence to Practice
○ External validity – can the results be applied to other populations, or more specifically, the patient in question?
○ Determine if the evidence is clinically significant, statistically significant, neither, or both
Through these steps, EBM incorporates interventions that work based on the high quality of evidence found, helps encourage communication among healthcare professionals, and facilitates the skill of research and keeping up with new information. However, that is not to say it is without its challenges or limitations. Individual patient factors must always be considered which may not always be synonymous with the evidence found, nor does EBM focus on explaining how the interventions are likely to work.
Making informed decisions in improving pharmacotherapy care is most effective through the utilization of EBM. Appropriate knowledge and skill are necessary to get the most out of it. EBM’s role in healthcare is inarguable, and it will continue to make an impact for years to come.
Midrara Kashmari
RxPharmacist Team
References:
- Chant C. Evidence-Based Pharmacy Practice? The Canadian Journal of Hospital Pharmacy. 2017;70(4). doi:https://doi.org/10.4212/cjhp.v70i4.1673.
- Aparasu RR, Bentley JP. Principles of Research Design and Drug Literature Evaluation. Jones & Bartlett Learning; 2015.
- The Pharmacist’s Guide to Evidence-Based Medicine for Clinical Decision Making. ASHP. https://www.ashp.org/-/media/store-files/p1770-sample-chapter-1.
- Wagner K. Research Guides: Introduction to Evidence-Based Practice: Overview. guides.lndlibrary.org. https://guides.lndlibrary.org/c.php?g=705624&p=5011032
- Straus SE, Glasziou P, Warren Scott Richardson, R. Brian Haynes. Evidence-Based Medicine.; 2019.