“Now remember to complete the entire course of your antibiotic until it’s finished, even if you feel better.”
How often has a patient heard this from either their doctor or pharmacist? Hopefully every time. As vital drugs, antibiotics have saved countless lives. Akin to other drugs, they can also be misused or overused. However, what sets them apart as a class of drugs is the unique threat that comes with their use: antibiotic resistance. Why is that a threat?
Understanding Antibiotic Resistance
Antibiotic resistance refers to the ability of microorganisms such as bacteria to continue to grow and ultimately defeat the very drug (antibiotic) intended to limit their growth or kill them altogether.1 In other words, the microorganism becomes resistant to the antibiotic treatment. Eventually, resistance of the microorganism to even one drug poses a risk to other drugs in the same class. When this occurs, infections become harder and harder to treat.
Now why this occurs is because bacteria can adapt and develop resistance through natural selection by the mere presence of antibiotics. The purpose of antibiotics is to kill bacteria, regardless of if they’re the bad bacteria that cause infection or the good bacteria that protect us from infection. Killing the good bacteria would cause loss of the protection that they normally provide allowing the bad bacteria to grow. What could make this worse?
Factors Contributing to Antibiotic Resistance
- Incomplete courses of antibiotic treatment → by not finishing the entire course, bacteria that survived become resistant and multiply or pass on their resistant genes to other surviving bacteria
- Inappropriate prescribing of an antibiotic → using an inappropriate antibiotic drug that wouldn’t effectively treat the infection or using antibiotics when not needed allows bacteria to spread and either worsen or cause an infection
- Overprescribing of antibiotics → increased use of antibiotics gives bacteria more chances to grow, survive, and become resistant through multiple mechanisms of current and future antibiotics
The Consequences
If antibiotic resistance develops to the point of utilizing first-line treatment options, then use of second or third-line options may become necessary. However, they are not always ideal or as effective, and prolonged drug treatment use may cause serious side effects and may lead to a delay in recovery. In addition, some patients with chronic conditions may not have a strong immune system to fight off simple infections, much less infections from resistant bacteria. In addition, it is possible that in some cases there are not any more treatment options to continue. All these aspects contribute to increased healthcare costs, decreased effectiveness of interventions, and poor health outcomes for patients.
Pharmacists and Antibiotic Stewardship
Pharmacists play a vital role in promoting responsible, appropriate, and effective antibiotic use. Some interventions performed by pharmacists involve dose adjustments, dose optimization (increasing or decreasing the dose depending on patient’s health status), drug-interactions, stop orders that are time sensitive, changing IV antibiotics to oral formulation, and removing or discontinuing duplicate antibiotic therapy.3
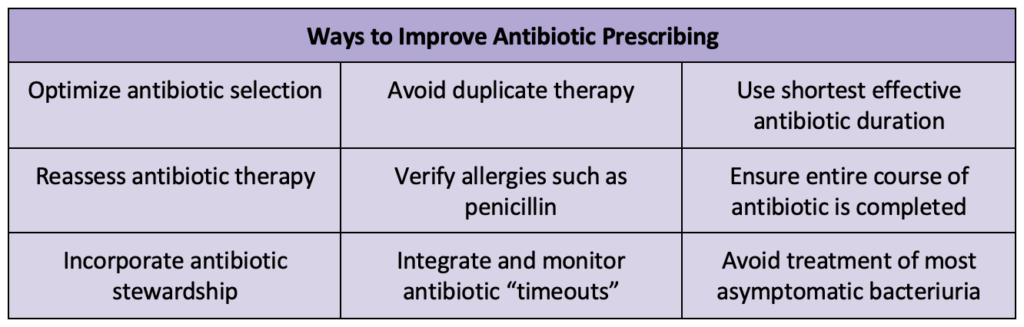
Antibiotic resistance is a multifaceted challenge. Pharmacists have a vital role in educating patients, promoting responsible antibiotic use, and advocating for evidence-based prescribing practices. Their knowledge and skills allow them to provide education to both patients and other healthcare providers regarding adherence, drug dosing, and proper antibiotic use. Through collaboration with providers, proper and effective antibiotic use can improve and continue for all current and future generations.
Midrara Kashmari
RxPharmacist Team
References:
- Centers for Disease Control and Prevention. About Antimicrobial Resistance. CDC. Published March 13, 2020. https://www.cdc.gov/drugresistance/about.html.
- Centers for Disease Control and Prevention. How Antibiotic Resistance Happens. CDC. Published October 5, 2022. https://www.cdc.gov/drugresistance/about/how-resistance-happens.html.
- Centers for Disease Control and Prevention. Core elements of hospital antibiotic stewardship programs. CDC. Published 2019. https://www.cdc.gov/antibiotic-use/core-elements/hospital.html.
- Chan AHY, Beyene K, Tuck C, Rutter V, Ashiru-Oredope D. Pharmacist beliefs about antimicrobial resistance and impacts on antibiotic supply: a multinational survey. JAC-Antimicrobial Resistance. 2022;4(4). doi:https://doi.org/10.1093/jacamr/dlac062.

