
Pneumonia is a lung infection caused by bacteria, fungi, or viruses. Pneumonia is the leading cause of infection-related death and the 8th most common cause of death worldwide. In the United States, the incidence of community-acquired pneumonia (CAP) is 24.8 cases for every 10,000 adults. Hospital-acquired pneumonia (HAP) occurs in 5-10 of every 1000 hospital admissions, making it the most common infection caused by hospitalization. Antibiotics are the mainstay of pneumonia treatment, and choosing the correct antibiotic depends on various factors. Pharmacists can impact patient care by ensuring that patients receive the most appropriate therapy.
What are CAP and HAP?
Pneumonia is classified by the environment in which the infection occurred and how severe the disease is. Both classifications help to determine treatment options.
CAP is a pneumonia infection that is acquired outside of the hospital. If patients are hospitalized, it is present within the first 48 hours of hospitalization and will show up on initial cultures taken at the time of admission. CAP is the most common type of pneumonia.
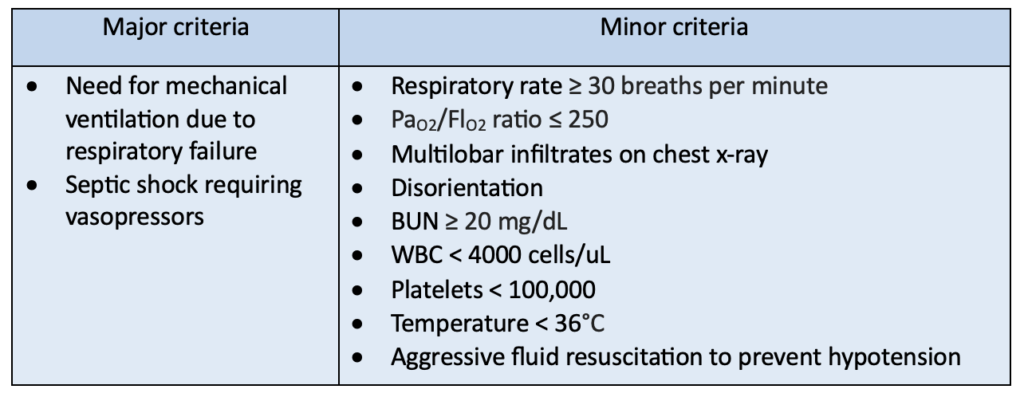
CAP severity is part of the initial patient assessment to determine if a patient should be treated in an inpatient or outpatient setting. Generally, severe CAP is classified as a case with 1 or more major criteria or 3 or more minor criteria.
HAP is a pneumonia infection that is acquired during a hospital stay. It occurs after a patient has been hospitalized for more than 48 hours and is not present on initial cultures upon admission. HAP is less common than CAP but generally requires more robust treatment, which takes place in the hospital.
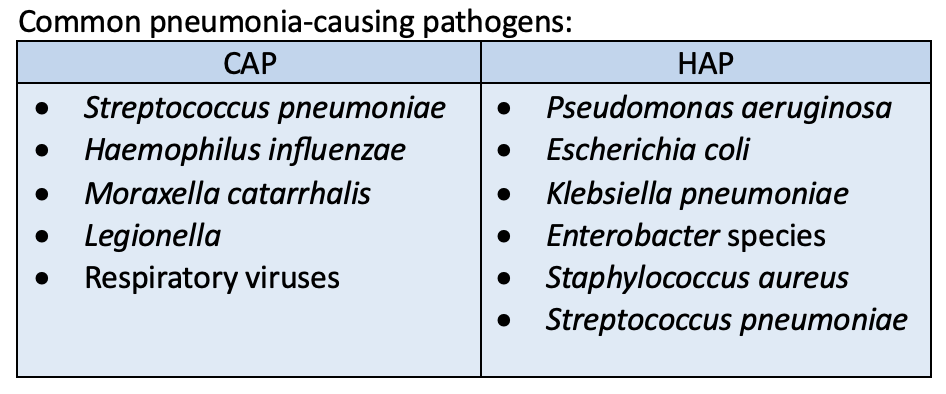
Pathogens that cause CAP and HAP
Pathogens causing pneumonia vary; some pathogens are more common in healthcare settings, while others are more common in everyday environments. Additionally, local infection and resistance patterns for infectious organisms can cause variation in pneumonia pathogens.
What are the signs and symptoms of pneumonia?
Many of the signs and symptoms of pneumonia are consistent with other infections. No single sign or symptom should be used to diagnose pneumonia. Similarly, the lack of a specific sign or symptom should not be used on its own to rule out pneumonia.
Common symptoms of pneumonia include:
- Fever
- Chills
- Chest pain
- Cough with sputum production
- Shortness of breath
Physical exam and lab findings:
- Increased heart rate
- Respiratory rate > 20 breaths per minute
- Elevated white blood cells (WBC)
- Lung crackles or decreased breath sounds
How is pneumonia diagnosed?
Chest X-ray is the gold-standard diagnostic test for patients with suspected pneumonia. The combination of an infiltrate on a chest x-ray and presence of clinical signs and symptoms is indicative of pneumonia and warrants empiric antibiotic treatment.
Respiratory cultures are the main laboratory evaluation used to diagnose pneumonia. However, they can be invasive and easily contaminated. They can be obtained through sputum samples, endotracheal aspiration, and bronchoscopy. Respiratory cultures are not required to diagnose pneumonia and are not commonly performed for patients with non-severe CAP. For patients with more serious infections, including severe CAP and HAP, respiratory cultures can help narrow antibiotic coverage and ensure that uncommon pathogens are appropriately covered by antibiotics.
Treatment for CAP and HAP
Antibiotics should be used to treat patients diagnosed with pneumonia. Pneumonia severity, causative pathogen, and local resistance rates should all be taken into consideration when choosing antibiotics from the treatment guidelines. Additionally, patient-specific factors such as allergies, previous infections, and previous antibiotic use should be considered before starting antibiotics.
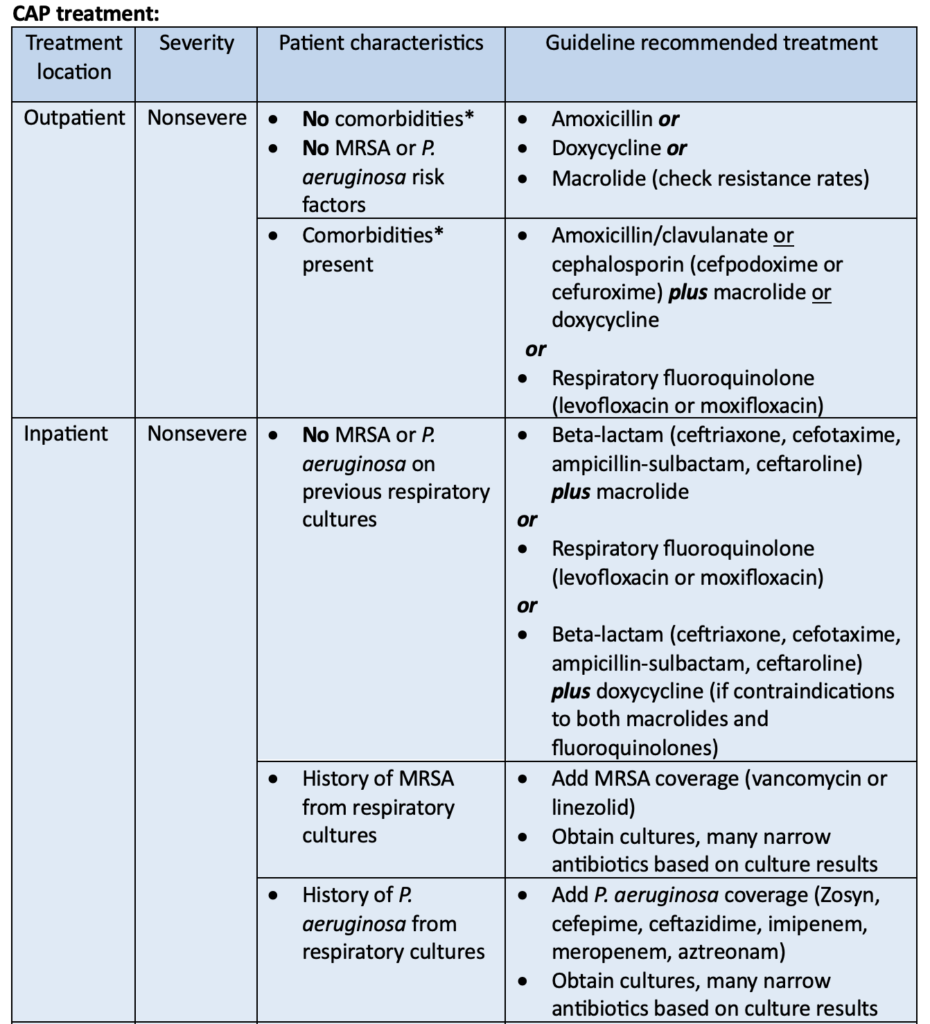
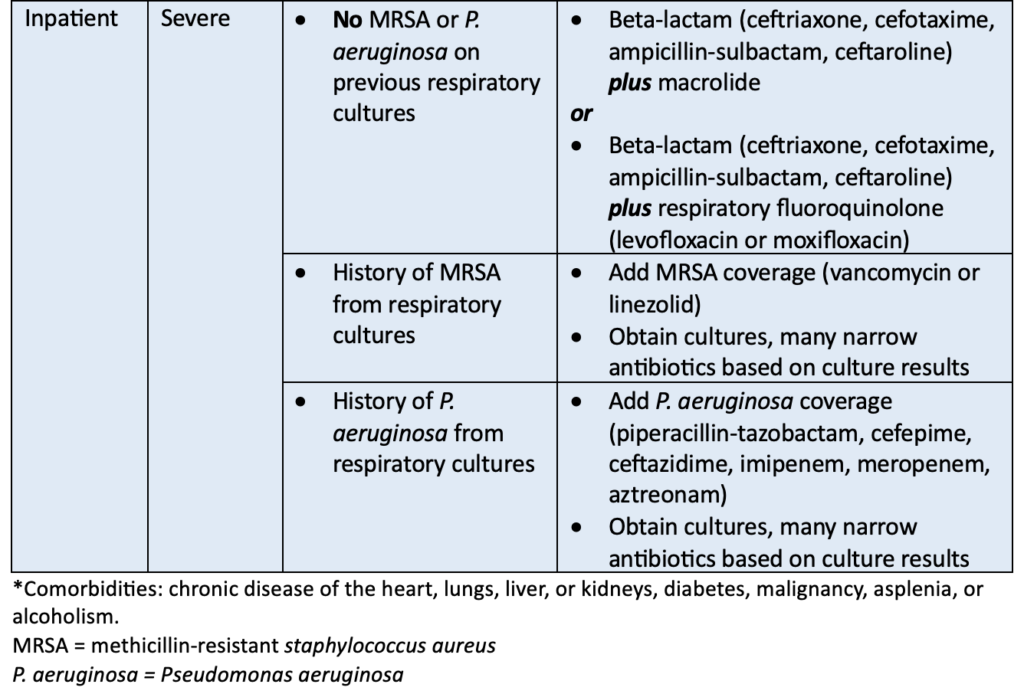
Treatment for CAP should be continued until the patient is clinically stable and antibiotics have been given for at least 5 days. Clinical stability includes signs that the patient is recovering such as normal heart and respiratory rates, no fever, willingness to eat, stable blood pressure, and normal mental status. The duration of antibiotic treatment may be extended if the patient does not show signs of improvement or the causative pathogen is uncommon and more difficult to treat.
HAP treatment:
All patients who are diagnosed with HAP should be treated with at least 1 antibiotic. This antibiotic should cover P. aeruginosa and methicillin-susceptible staphylococcus aureus (MSSA). Additional MRSA and P. aeruginosa coverage may be indicated for specific patient populations. The table below outlines the guideline-recommended antibiotics for HAP and when additional antibiotic coverage is necessary.
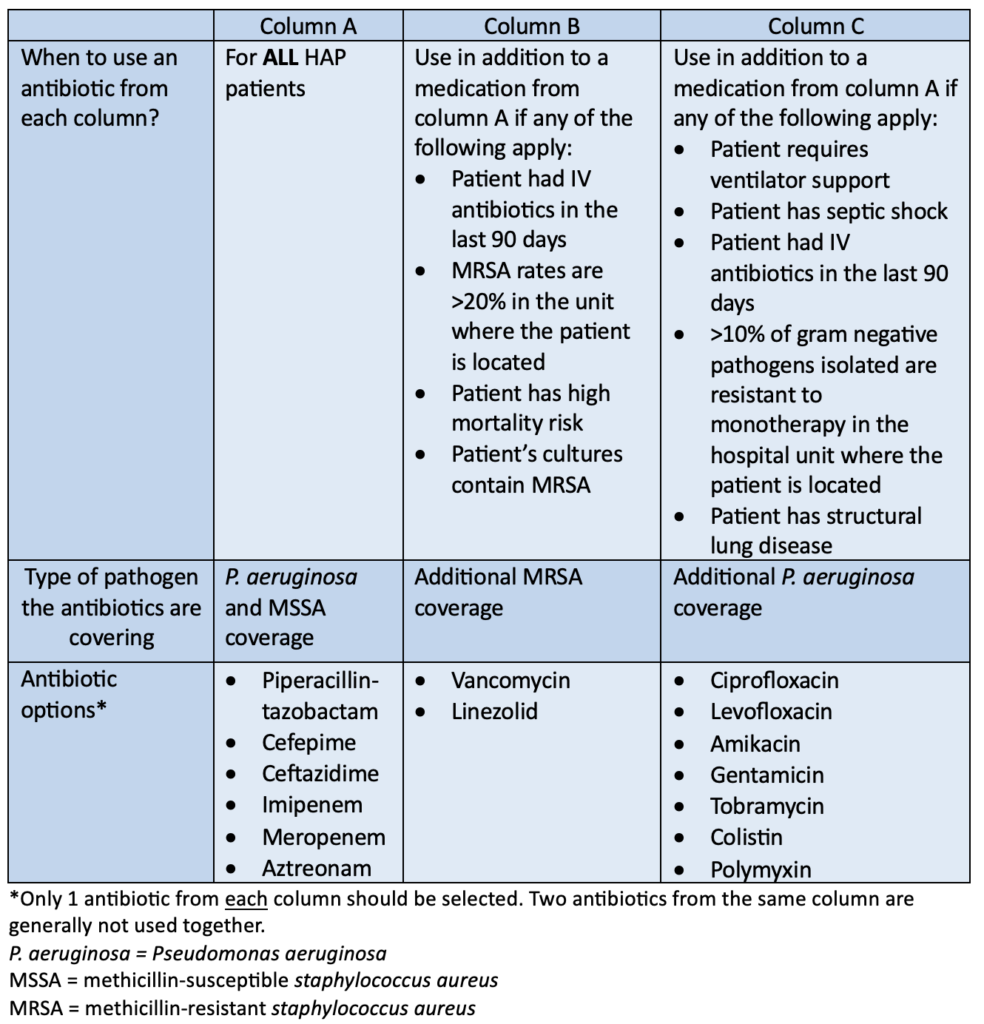
Antibiotics should be narrowed to treat the causative pathogen as soon as possible. Treatment for HAP should be limited to 7 days as long as the patient is clinically improving. Clinical improvement may include a reduction in symptoms, normalized heart and respiratory rates, discontinuation of vasopressors and ventilation, and improved oxygen saturation. Antibiotics may be given for a longer duration if the patient is not clinically improving.
Viral pneumonia treatment
Viral pneumonia is rare and hard to diagnose. The main treatments for viral pneumonia are supportive care and management of precipitating infections.
Supportive care may include:
- Supplemental oxygen
- Oral or IV fluids
- Frequent meals
- Rest
Viral infections, such as influenza or respiratory syncytial virus, are the main cause of viral pneumonia. Therefore, giving antiviral medications to treat current viral infections is recommended to help speed up viral pneumonia recovery.
Fungal pneumonia treatment:
Fungal pneumonia is caused by inhaled fungal spores. It is more common in people with weakened immune systems such as organ transplant recipients, cancer patients, and the elderly. Fungal pneumonia is often treated with antifungal medications given either by mouth or IV.
Antifungal medications used:
- Itraconazole
- Fluconazole
- Amphotericin B
How can pharmacists help?
Pneumonia is a common infection caused by a variety of pathogens. It affects a large number of people each year and is classified as community-acquired or hospital-acquired. The main treatment for pneumonia is antibiotics. Pharmacists have in-depth knowledge of antibiotics and should use that knowledge to ensure that patients with pneumonia receive optimal medications to recover promptly.
Margaret M., APPE Student
References:
- Community-Acquired Pneumonia. National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/books/NBK430749/. Accessed August 26, 2024.
- Pneumonia. National Heart, Lung, and Blood Institute. Available at: https://www.nhlbi.nih.gov/health/pneumonia. Accessed August 26, 2024.
- Nosocomial Pneumonia. National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/books/NBK535441/. Accessed August 26, 2024.
- Guidelines for Diagnosis and Treatment of Adults with Community-Acquired Pneumonia. Infectious Disease Society of America. Available at: https://www.idsociety.org/practice-guideline/community-acquired-pneumonia-cap-in-adults/. Accessed August 26, 2024.
- 2016 Clinical Practice Guidelines for the Management of Adults with Hospital-acquired and Ventilator-associated Pneumonia. Infectious Disease Society of America. Available at: https://www.idsociety.org/practice-guideline/hap_vap/. Accessed August 26, 2024.
- Viral Pneumonia. National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/books/NBK513286/. Accessed August 27, 2024.
- Systemic Antifungal Therapy for Invasive Pulmonary Infections. Journal of Fungi. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9966409/. Accessed August 27, 2024.
