GLP-1 receptor agonists (GLP-1s) have become a hot topic in recent years. Celebrities, online influencers, and even multi-billionaires like Elon Musk use them, touting them as a quick fix weight loss solution. With about 70% of American adults being overweight or obese, and many dealing with related health complications, it’s no surprise that people seeking a slimmer figure are turning to GLP-1s for help. After all, the ability to lose upwards of 10-25 pounds just by taking a weekly injection sounds ideal and convenient.
However, GLP-1s are more than just a trend. It is a class of drugs used as a second-line add-on medication in type 2 diabetes management and as a first-line treatment in obesity management. This growing popularity, especially among those with obesity, has contributed to a nationwide drug shortage and raises concerns about ensuring that patients with diabetes still have access to these vital treatments. Therefore, understanding the appropriate use of GLP-1s for individuals is crucial.
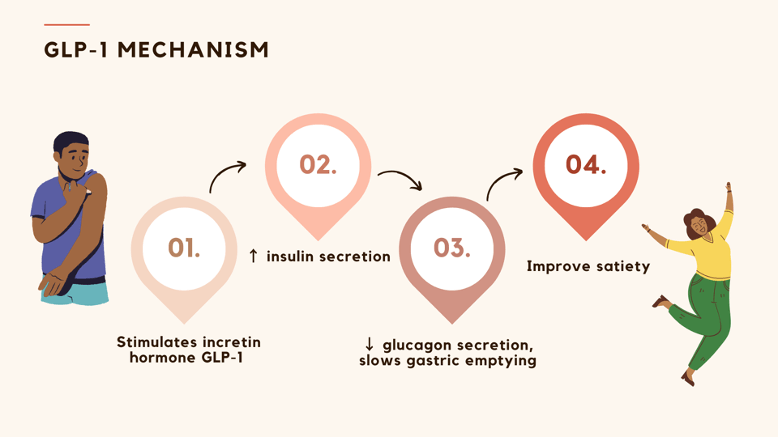
How do GLP-1s work?
GLP-1s work by stimulating insulin secretion and suppressing glucagon secretion in hyperglycemic states. This delays gastric emptying and decreases appetite.
What are GLP-1s used for?
- Diabetes Mellitus
GLP-1s are primarily used as a second-line treatment for type 2 diabetes. They are especially beneficial when used alongside metformin or combination therapy in the following situations:
- Atherosclerotic cardiovascular disease (ASCVD)
- Chronic kidney disease (if SGLT2 inhibitors are not tolerable or if additional glucose control is needed)
- Existing combination therapy with need for additional weight loss or glycemic management
- Weight Loss
GLP-1s are also a first-line therapy for managing obesity in patients who have not achieved at least 5% total body weight loss in three to six months through lifestyle interventions. They are recommended for:
- Individuals with a BMI >30 kg/m²
- Individuals with a BMI of 27-29.9 kg/m² who have weight-related comorbidities such as hypertension, dyslipidemia, type 2 diabetes mellitus, obstructive sleep apnea, or cardiovascular disease
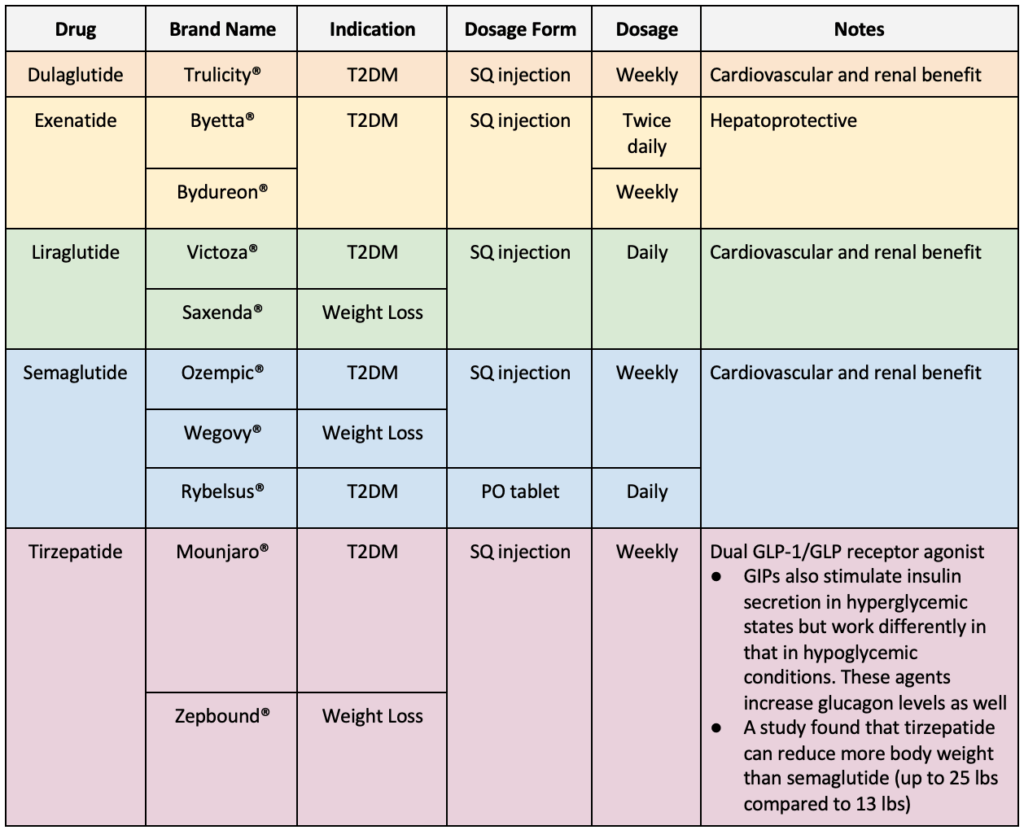
See below for additional information regarding available GLP-1 medications:
What are some adverse reactions and warnings to be aware of?
When starting GLP-1 receptor agonists, patients typically undergo a titration period to help mitigate gastrointestinal side effects. It is recommended to prescribe a low dose initially and gradually increase it to minimize adverse effects like nausea and vomiting.
- Gastrointestinal (nausea, vomiting, diarrhea)
- Injection site reactions (redness, itching, swelling)
- Acute kidney injury
- Cholelithiasis (gallstones)
Black Box Warning
GLP-1s are not recommended in patients with or at risk of Thyroid C-Cell tumors. These drugs are also not recommended for pregnant patients and those with severe gastrointestinal diseases (ulcerative colitis, Crohn’s disease, irritable bowel syndrome, inflammatory bowel disease).
Challenges
Despite their effectiveness, GLP-1s face challenges regarding cost and availability. A one-month supply of these medications can cost over $1,000 without insurance, creating a financial barrier for many people. The demand for these drugs has also exceeded supply, causing major manufacturers to announce shortages. The Food and Drug Administration (FDA) manages a website that allows healthcare providers and patients to view drugs on shortage. To further assist patients, a telehealth company, Ro, has also developed a public tracker to provide real-time availability information submitted by consumers themselves. Another issue to note is the disparity in medication access, with the largest users being disproportionately non-Hispanic white females. Difficulty finding insurance coverage further exacerbates these inequities. Lastly, counterfeit versions of GLP-1s have also emerged in the market, posing risks to patient safety. Addressing these issues requires collaborative effort between insurers, healthcare professionals, and government entities to improve access, lower costs, and to ensure the authenticity and safety of medications.
Takeaway
GLP-1s offer significant benefits for diabetes and obesity management, but challenges such as high costs and shortages limit access to patients who need the drugs. People who are seeking these medications should always see a licensed medical professional to determine if the use of GLP-1s is the most appropriate option for them. Healthcare providers and pharmacists alike have a responsibility to stay informed about these medications, their availability, and cost to ensure they can offer the best guidance for patients.
Winnie Chu
RxPharmacist Team
Resources
- Tirzepatide versus Semaglutide Once Weekly in Patients with Type 2 Diabetes. The New England Journal of Medicine. 2021;385(6):503-515. doi:10.1056/NEJMoa2107519. Available at: https://www.nejm.org/doi/full/10.1056/NEJMoa2107519. Accessed August 3, 2024.
- FDA Approves New Medication for Chronic Weight Management. U.S. Food and Drug Administration. Available at: https://www.fda.gov/news-events/press-announcements/fda-approves-new-medication-chronic-weight-management. Accessed August 3, 2024.
- Glucagon-like peptide-1 receptor agonists. Available at: https://www.ncbi.nlm.nih.gov/books/NBK551568/. Accessed August 3, 2024.
- Shifting Trends in the Indication of Glucagon-like Peptide-1 Receptor Agonist Prescriptions: A Nationwide Analysis. Available at: https://www.acpjournals.org/doi/10.7326/M24-0019. Accessed August 3, 2024.
- Are You Sure Your Ozempic Is Real? Fakes Are on the Rise. The New York Times. July 12, 2024. Available at: https://www.nytimes.com/2024/07/12/well/ozempic-fake-counterfeit-drugs.html. Accessed August 3, 2024.
- Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2024. American Diabetes Association. 2024;26(4):501-510. doi:10.1111/dom.14535. Available at: https://pubmed.ncbi.nlm.nih.gov/38078590/. Accessed August 3, 2024.
