
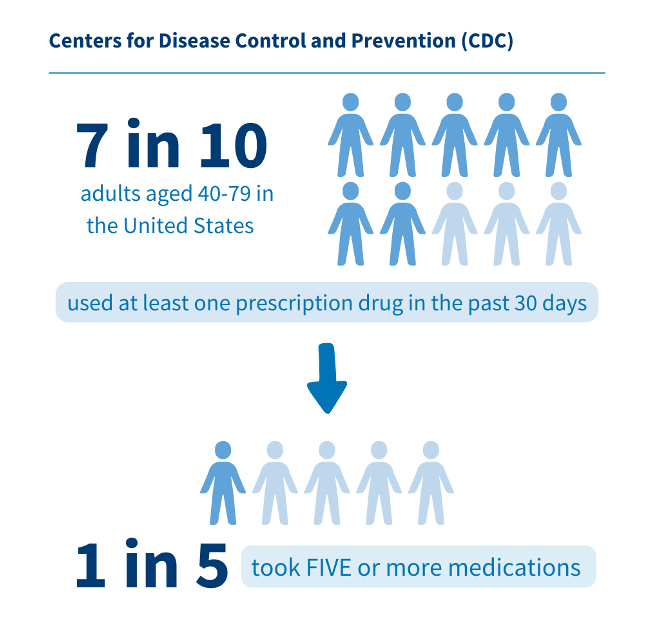
Do you know someone who is overwhelmed with managing multiple medications? Maybe you know a close relative or have even seen this happening in practice settings. These experiences may be due to polypharmacy, and it’s a growing concern, especially among older adults. Polypharmacy refers to the use of several medications, typically five or more, daily. It is common in individuals with multiple chronic conditions, such as arthritis, asthma, diabetes, or hypertension. According to the Centers for Disease Control and Prevention (CDC), 7 in 10 adults aged 40-79 in the United States used at least one prescription drug in the past 30 days, and around 1 in 5 took five or more prescription drugs. While polypharmacy can help manage complex health issues, it also raises safety concerns, making pharmacists essential in ensuring safe medication use.
As you can imagine, taking so many medications daily can pose health risks for the patient. Here’s why polypharmacy can be a significant concern:
- Complex Medical System
Older adults frequently manage several chronic conditions, which leads to polypharmacy. This often involves various medications prescribed by multiple doctors, sometimes filled at different pharmacies. This makes it difficult to track what they are taking at one time.
- Tracking and Management
Keeping up with multiple medications can be difficult with all the pills, varying dosages, and times of administration. This often leads to trouble with medication adherence and can result in missed doses or improper medication use, further complicating health management.
- Increased Risk of Adverse Reactions
The use of excessive or unnecessary medications can increase the risk of experiencing adverse drug reactions and drug interactions. This risk is particularly significant in the aging population, as changes in body composition and metabolism can affect how medications are absorbed, distributed, and eliminated. As a result, older adults are more susceptible to side effects and unintended consequences from their medications.
- Increased Health Costs
Polypharmacy can lead to adverse effects that may require hospitalization. If not managed properly, this can trigger a prescribing cascade, where a side effect of one medication is misdiagnosed as a new condition and treated with additional medications. This cycle can have serious health consequences, increasing both the patient’s care costs and the likelihood of repeated hospitalizations. The added burden of managing these issues also increases expenses for the healthcare system.
Often, these issues are preventable. Healthcare professionals, particularly pharmacists, play a crucial role in managing medications and preventing such complications. The World Health Organization (WHO) outlines the following key steps for ensuring medication safety:
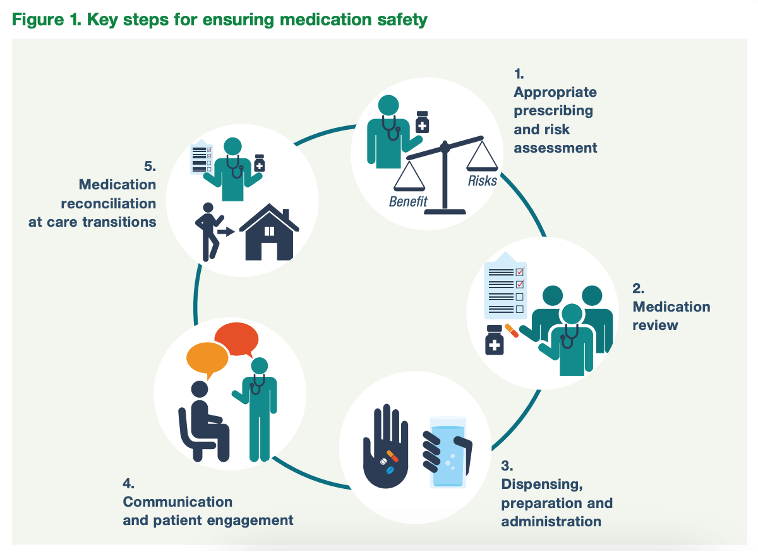
As the figure describes, medications should be reviewed for appropriate prescribing. A helpful resource that assists with evaluating medication risks in elderly patients is the American Geriatrics Society Beers Criteria®. The AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults is updated every three years and provides a list of medications to be used cautiously or avoided in older adults. This includes drugs generally inappropriate, those to avoid in specific conditions, those to use cautiously, drug-drug interactions, and dose adjustments based on kidney function.
Other ways pharmacists can be involved in a patient’s medication management include encouraging patients to maintain an up-to-date list of all their medications, including prescriptions, over-the-counter drugs, and supplements. This list should be shared with healthcare providers to identify potential side effects and interactions. Patients and caregivers should be counseled on common side effects to watch for. These commonly include:
- Headaches and confusion
- Dizziness and falls
- Weight changes
- Memory or cognitive issues
Encouraging regular checkups and having all prescriptions filled at one pharmacy can help pharmacists monitor for potential drug interactions and manage medications more effectively. If necessary, they can coordinate with physicians to review medications and explore safer alternatives for the patient. Furthermore, the patient may consult a pharmacist before purchasing any over-the-counter product or supplement to ensure safety with current medications or health conditions. Medication reconciliation during transition of care settings further supports safe medication use by addressing any inconsistencies and errors in medication lists as the patient moves between different care settings.
All in all, while taking multiple medications has its risks, it can also happen out of necessity, such as in patients with diabetes who may require multiple medications. As a result, it is crucial to manage and monitor it carefully. Regular check-ups and clear communication about medications can help mitigate the risks associated with taking multiple drugs. Deprescribing also needs to be approached carefully, as stopping certain medications can lead to withdrawal effects or exacerbate existing conditions. The objective is to minimize inappropriate polypharmacy where too many medications are prescribed inappropriately, while ensuring that the use of multiple medications is truly beneficial for the patient’s health. By focusing on effective management and informed patient care, we can make reduce polypharmacy and improve health outcomes.
Winnie Chu
RxPharmacist Team
Resources
- National Center for Biotechnology Information. Polypharmacy: A Case Report and Clinical Review. Available at: https://www.ncbi.nlm.nih.gov/books/NBK532953/. Accessed July 24, 2024.
- National Institute on Aging. The Dangers of Polypharmacy and the Case for Deprescribing in Older Adults. Available at: https://www.nia.nih.gov/news/dangers-polypharmacy-and-case-deprescribing-older-adults. Accessed July 24, 2024.
- World Health Organization. Medication Safety in Polypharmacy. Available at: https://www.who.int/docs/default-source/patient-safety/who-uhc-sds-2019-11-eng.pdf. Accessed July 24, 2024.
- Centers for Disease Control and Prevention. Prescription Drug Use Among Adults Aged 40–79 in the United States and Canada. Available at: https://www.cdc.gov/nchs/products/databriefs/db347.htm. Accessed July 24, 2024.
