Urinary tract infection (UTI) is a broad term, encompassing simple and complex infections of the urinary tract and kidneys. In the United States, 40% of women have at least one UTI in their lifetime. Antimicrobials are the main treatment used for UTIs, but selecting the most appropriate option is complicated by increased resistance rates and patient-specific factors. Pharmacists play an important role in the healthcare team by ensuring that antimicrobial selection is optimal for each patient.
Cystitis vs. pyelonephritis
Cystitis is a UTI, consisting of a bladder or lower urinary tract infection. This is the most common type of UTI and one of the most common indications for prescribing antimicrobials in the United States.
Cystitis can be classified as complicated or uncomplicated.
- Uncomplicated cystitis is any UTI that occurs in women who are generally healthy and do not have any abnormalities in the structure or function of their urinary tract.
- Complicated cystitis is any UTI that occurs in people who have abnormalities to the structure or function of their urinary tract or have other complicating health problems.
- UTIs that occur in men or pregnant women are always considered complicated.
Pyelonephritis is a complicated UTI that involves infection of the kidneys or upper urinary tract. This is less common than cystitis and requires more intense treatment.
Who gets UTIs?
Women are 4 times more likely to get a UTI than men. This is due to women having shorter urethras, and a shorter space between the rectum and urethra, both of which allow bacteria to travel more easily to the site of infection. Cystitis occurs most frequently in women ages 16 to 35 but can happen to anyone at any age. Pyelonephritis occurs in about 15-17 cases per 10,000 females and 3-4 cases per 10,000 males each year. In the United States, an average of 250,000 cases of pyelonephritis occur each year.
Some additional risk factors include:
- Abnormal function or anatomy of the urinary tract
- Antibiotic use
- Diabetes
- Diarrhea
- First UTI before age 15
- New or multiple sexual partners
- Menopause
- Pregnancy
- Old age or dementia
- Catheter-use
What causes UTI?
Common pathogens that cause cystitis and pyelonephritis are:
- Escherichia coli
- Proteus mirabilia
- Klebsiella pneumonias
- Staphylococcus saprophyticus
- Enterococcus
E. coli is the most common pathogen in UTIs, responsible for 75-95% of infections. One possible mechanism for the success of E. coli is the p-fimbriae appendages that adhere to epithelial cells in the urinary tract. This can prevent E. coli from being flushed out of the urinary tract, instead giving them time to colonize and spread.
UTI symptoms and diagnosis
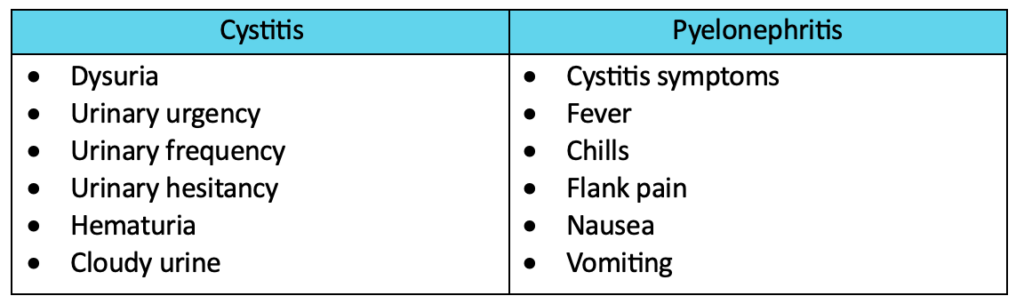
Many cystitis symptoms overlap with other urinary tract diagnoses. Likewise, many pyelonephritis symptoms overlap with other types of infections. Therefore, it is important to collect a medical history and a full list of reported symptoms from each patient who presents with a possible UTI.
Diagnosis of UTI is made using a combination of patient-reported symptoms, a detailed medical history, and a urinalysis. No single factor alone should be used to diagnose UTIs.
Treatment for UTIs
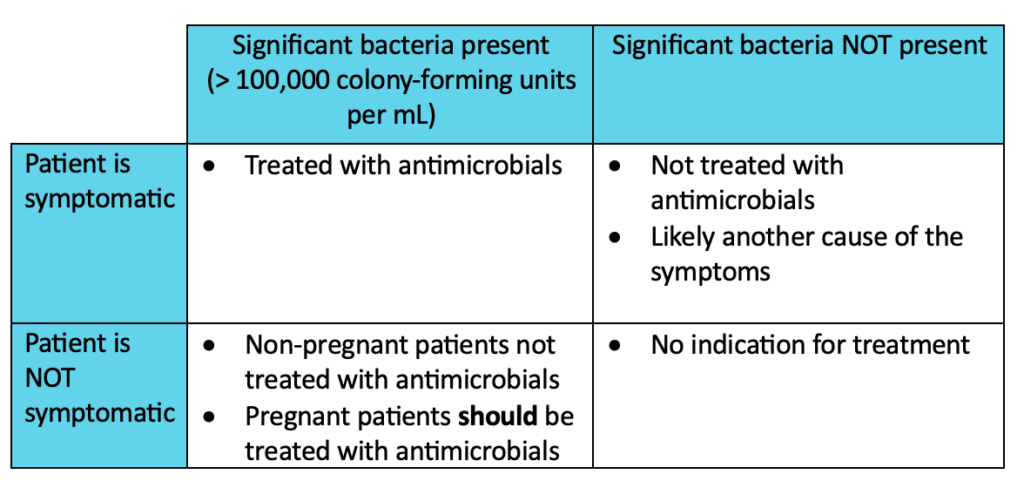
Antimicrobial agents are the main medications used to treat UTIs. However, the agent selected and treatment duration differ between cystitis and pyelonephritis. Medication selection should be patient-specific, taking into consideration previous antimicrobial use, history of UTIs, cost, availability, and allergies. Antimicrobial selection should also be location-specific, taking into consideration local resistance patterns.
Antimicrobial treatment is dependent on the presence of symptoms and significant bacteria in the urine sample. A notable exception is the treatment of pregnant women. All pregnant patients who have significant bacteria present in their urine should be treated with antimicrobials whether they have symptoms or not.
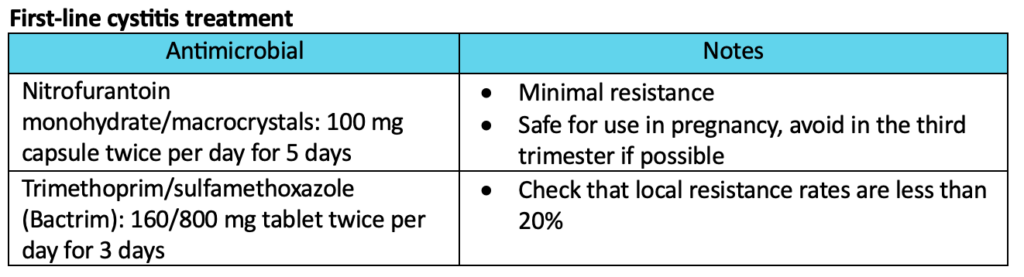
Cystitis treatment:
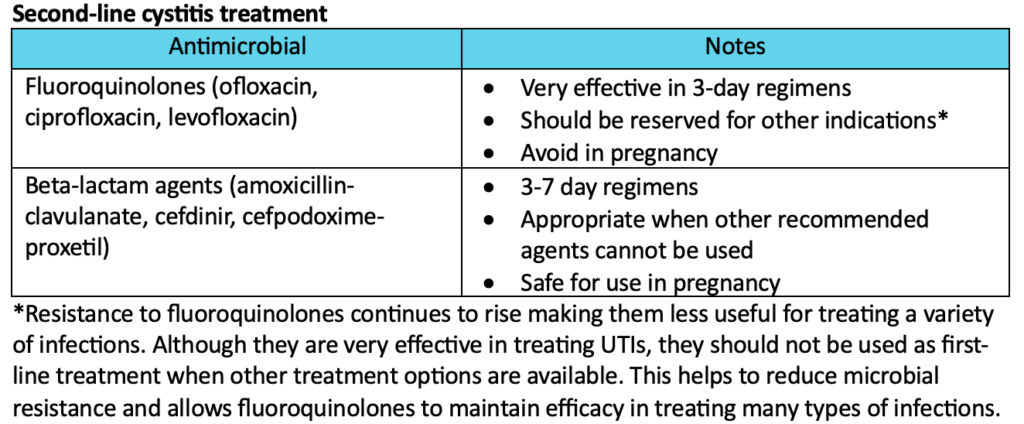
Cystitis treatment generally consists of a short course of oral antibiotics. There are multiple first-line options to choose from, all of which have similar efficacy. Second-line options are reserved for patients who cannot use any of the first-line treatments. Amoxicillin or ampicillin are NOT recommended due to poor efficacy and high resistance.
Pyelonephritis treatment
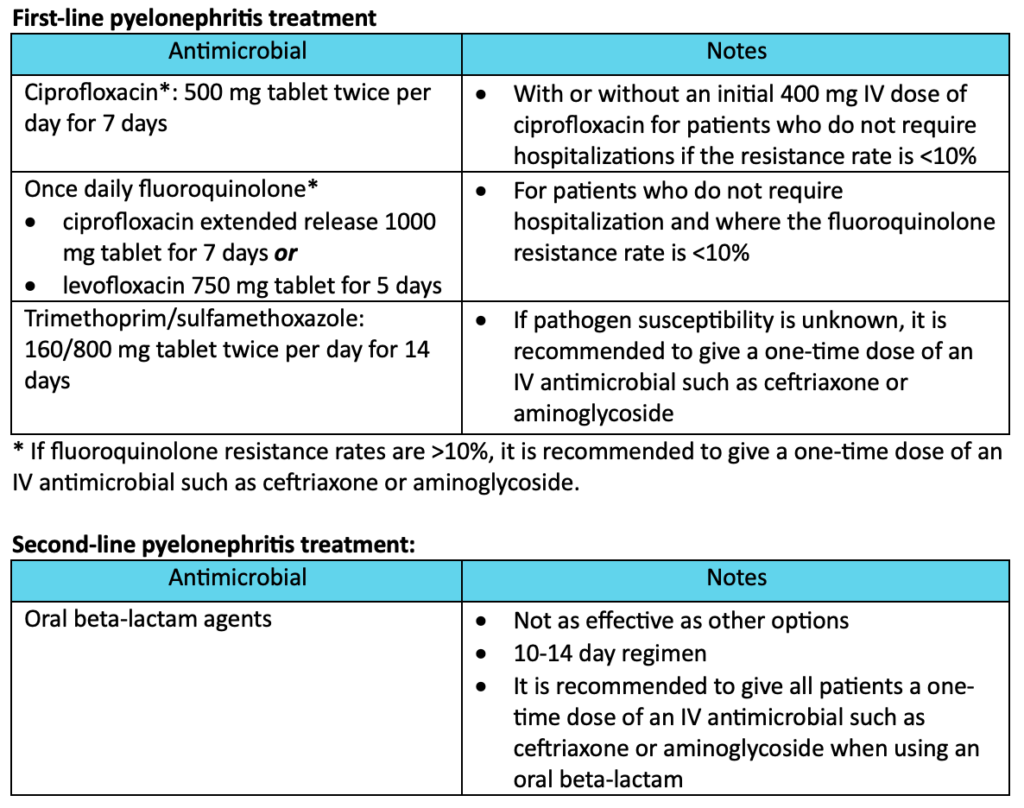
Pyelonephritis treatment generally uses longer courses of oral antimicrobials but may include IV treatment as well. Treatment may take place in the hospital or the outpatient setting depending on the severity of infection. If hospitalization is needed, patients should receive IV antimicrobials initially, then switch to oral treatment. If the patient is treated in the outpatient setting, they may use oral antimicrobials for the full treatment duration. All pregnant patients with pyelonephritis should be treated with IV therapy using ceftriaxone, cefepime, ampicillin plus gentamycin, or aztreonam.
Why is antimicrobial resistance a growing concern?
Antimicrobial resistance occurs when pathogens no longer respond to treatment with specific antimicrobial medications. In these cases, providers are required to prescribe alternative treatments that are not as specific and may come with additional side effects. A study from 2020 found that 1 in 5 UTIs caused by E. coli had reduced susceptibility to first-line treatment options such as trimethoprim/sulfamethoxazole. As more pathogens become resistant to commonly used antimicrobial medications, they will be harder to treat and treatment options will become limited.
Infections that occur due to drug-resistant pathogens have a higher rate of recurrence. It is critical to optimize treatment and limit recurrence by selecting antimicrobials using culture results and local resistance patterns and following guideline recommendations for indication and duration of therapy whenever possible.
What does this mean for pharmacists?
Almost half of the women in the United States will have at least one UTI in their lifetime. This makes UTIs one of the most common problems that require antimicrobial treatment. Pharmacists should consider the treatment guidelines, local resistance rates, and patient-specific factors when making recommendations and verifying prescriptions for UTI treatment.
Margaret M., APPE Student
References:
- Uncomplicated Urinary Tract Infections. National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/books/NBK470195/. Accessed August 27, 2024.
- Acute Pyelonephritis. National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/books/NBK519537/. Accessed August 27, 2024.
- International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women. Infectious Disease Society of America. Available at: https://www.idsociety.org/practice-guideline/uncomplicated-cystitis-and-pyelonephritis-uti/. Accessed August 27, 2024.
- Urinary Tract Infection in Pregnancy. National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/books/NBK537047/. Accessed August 28, 2024.
- Antimicrobial resistance. World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance. Accessed August 28, 2024.
