Polycystic Ovary Syndrome: An Unseen Struggle for Many Women

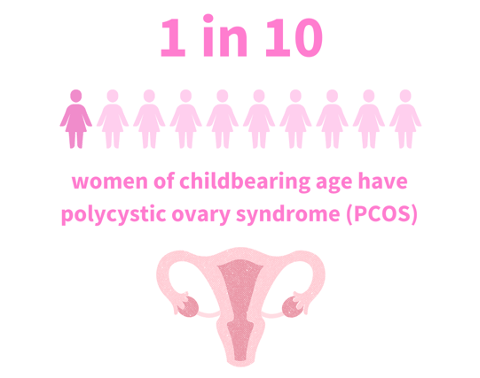
Despite affecting 1 in 10 women of childbearing age, polycystic ovary syndrome (PCOS) remains a common endocrine condition with many unanswered questions. While the disorder can significantly impact a woman’s health and fertility, it’s often under-recognized and misdiagnosed. A 2017 study highlights that over 50% of women with PCOS faced frustrating delays in diagnosis, sometimes over two years and involving more than three healthcare professionals. This leaves many undiagnosed women with ongoing concerns about managing symptoms like weight gain, irregular menstrual cycles, and infertility. Therefore, Increasing awareness and education among healthcare providers and improving patient support are crucial for enhancing outcomes and quality of life for those affected.
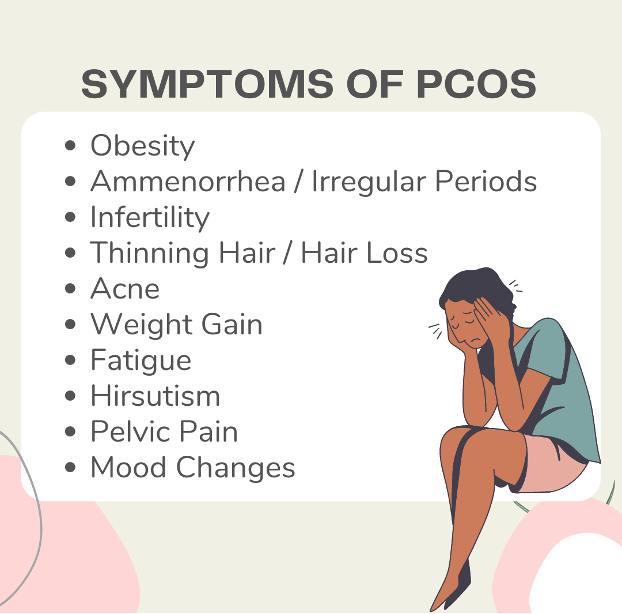
In addition to a myriad of symptoms, PCOS is linked to many other serious health risks that can further complicate a woman’s well-being. These include:
- Type 2 Diabetes
- Hypertension
- Lipid abnormalities
- Cardiovascular disease
- Obesity
- Sleep Apnea
- Depression
- Anxiety
- Endometrial Cancer
Diagnosis
Most women find out they have PCOS in their 20s and 30s when they have concerns with fertility and visit their healthcare provider. However, PCOS can present at any age after puberty. To properly diagnose PCOS, a woman must have two of the following symptoms:
- Irregular periods
- Elevated androgen levels
- Multiple cysts on one or both ovaries
Diagnosis typically involves several evaluations:
- Physical exam → includes measuring blood pressure, body mass index (BMI), and checking for symptoms such as excessive hair growth or hair loss
- Pelvic ultrasound (sonogram) → examines ovaries for cysts and the endometrial lining of the uterus
- Blood test → check androgen hormone levels, lipids, thyroid function to rule out other causative factors, and A1c and blood glucose levels
- Family history → the risk of PCOS is typically higher if an immediate family member, such as a sister, mom, aunt, also has a diagnosis
Cause
The exact cause of PCOS is not known, although several factors are thought to contribute. These include:
- Elevated levels of androgens
Elevated androgen levels can disrupt the ovarian cycle, leading to issues like anovulation (the absence of egg release), excessive hair growth, and acne
- Insulin resistance
Many women with PCOS do not respond properly to insulin and as a result, blood glucose is not absorbed efficiently within the body. This can increase glucose levels and over time increase the risk of type 2 diabetes.
Treatment
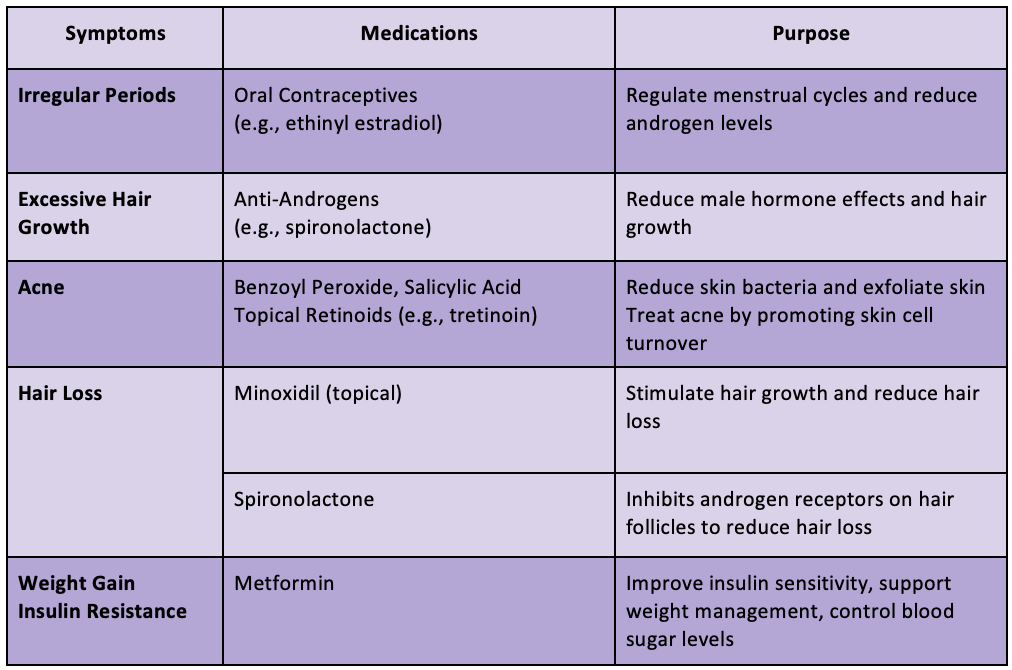
There is currently no cure nor any FDA-approved medications to treat PCOS. Symptoms are often managed through lifestyle interventions such as weight management, exercise, diet changes, or medications. See below for a comprehensive list of PCOS symptoms along with common first line off-label medication options.
Research and the Need for Action
Despite affecting 5 million women, PCOS remains severely underfunded and under-researched. Women with PCOS need treatments that address the condition’s root causes, not just its symptoms. Currently, only $10 million is allocated for PCOS research in 2024, and it is not included in recent major health funding initiatives. Consequently, this limited investment hinders the development of effective treatments.
There is hope, though. Spruce Biosciences is conducting the P.O.W.E.R study to assess if an investigational drug, tildacerfont, can effectively decrease androgen hormone production and improve PCOS symptoms. If successful, such breakthroughs could not only advance treatment options but also stimulate further research by demonstrating the condition’s relevance and significant impact on women’s health. With increased funding, these advances could significantly improve management and quality of life for those affected.
To conclude, PCOS remains a complex condition that is not completely understood. With its prevalence in women of childbearing age, it is only logical to push for more research in order to deepen our understanding and improve treatment options. Therefore, healthcare providers bear a responsibility to advocate for their patients to drive forward progress. By amplifying the voices of PCOS patients, we can drive meaningful change and improve outcomes for millions of women.
Winnie Chu
RxPharmacist Team
Resources
- Recommendations from the 2023 International Evidence-based Guideline for the Assessment and Management of Polycystic Ovary Syndrome. Fertility and Sterility. Available at: https://www.fertstert.org/article/S0015-0282(23)00719-7/fulltext. Accessed August 3, 2024.
- Polycystic Ovary Syndrome (PCOS). U.S. Department of Health and Human Services. Available at: https://www.womenshealth.gov/a-z-topics/polycystic-ovary-syndrome. Accessed August 3, 2024.
- Diabetes and Polycystic Ovary Syndrome (PCOS). Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/diabetes/risk-factors/pcos-polycystic-ovary-syndrome.html. Accessed August 3, 2024.
- Delayed Diagnosis and a Lack of Information Associated With Dissatisfaction in Women With Polycystic Ovary Syndrome. The Journal of Clinical Endocrinology & Metabolism. 2017;102(2):604-612. Available at: https://academic.oup.com/jcem/article/102/2/604/2972079. Accessed August 3, 2024.
- Polycystic Ovary Syndrome (PCOS) Research Program. Icahn School of Medicine at Mount Sinai. Available at: https://icahn.mssm.edu/research/pcos. Accessed August 3, 2024.
- P.O.W.E.R. Study. Spruce Biosciences. Available at: https://sprucebio.com/power/. Accessed August 3, 2024.
Polycystic Ovary Syndrome: An Unseen Struggle for Many Women Read More »
