Pharmacy Deserts: Navigating the Dry Lands of Medication Access

Imagine needing critical medication but having to travel miles to the nearest pharmacy. Or worse… finding none in your community. This scenario is a reality for 15.8 million Americans living in “pharmacy deserts.” Pharmacy deserts, modeled after the term “food desert,” describe areas where residents face significant barriers and have to travel considerable distances in order to access a pharmacy. It is a term coined in 2014 by Dr. Dima Qato, an associate professor at the University of Southern California studying pharmacy access and health equity. The distances defining this term varies depending on geographical location, as described below:
- Rural → Area within ten-mile radius from the nearest pharmacy
- Suburban → Area within two-mile radius from the nearest pharmacy, or half a mile for those without cars
- Urban → Area within one-mile radius from the nearest pharmacy, or half a mile for those without cars
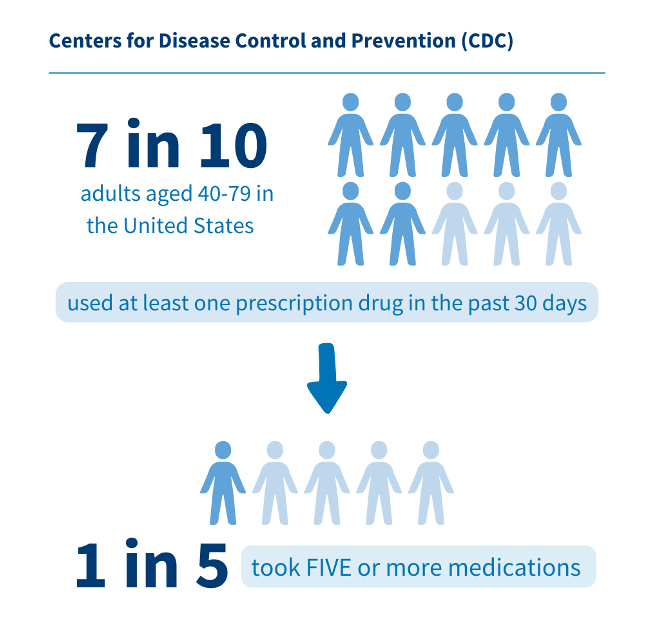
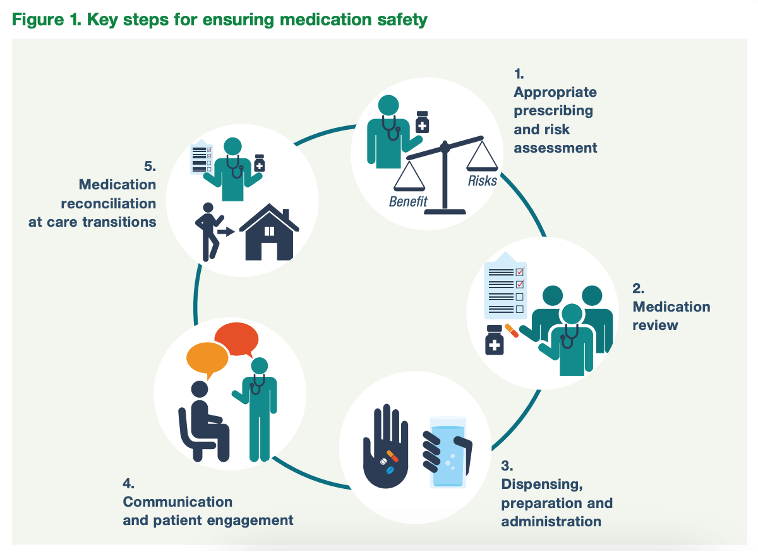
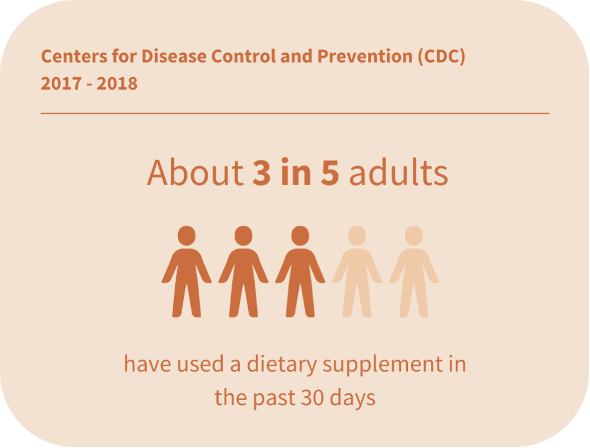
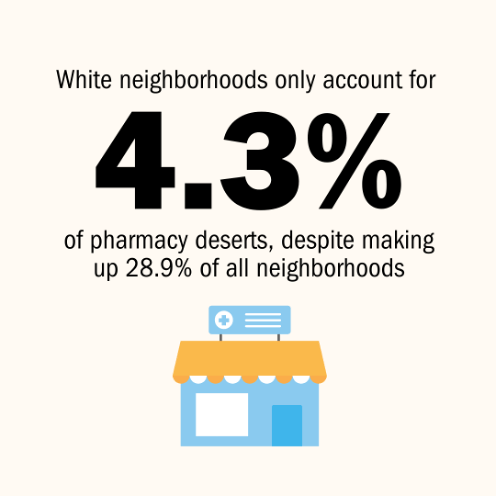
Pharmacists play a critical role in providing healthcare services and are often considered as the most accessible healthcare professionals. Aside from dispensing essential medications, pharmacists also assist in immunization administration and diagnostic testing. The consequences of not having a pharmacy within adequate traveling distance can affect many lives, particularly in marginalized communities, where they are most prevalent. Dr. Qato’s studies show that predominantly white neighborhoods, despite making up 28.9% of all neighborhoods, only account for 4.3% of pharmacy deserts. This highlights the uneven distribution of pharmacy resources, the need for improved pharmacy access in underserved areas, and the importance of providing medical care for those who need it the most.
Factors Contributing to Pharmacy Deserts and Impact
Grasping the underlying causes of pharmacy deserts is key to finding effective solutions. Various challenges contribute to the lack of pharmacy access in many communities.
Pharmacy Closures
In the past couple of years, there has been an increase in community pharmacy closures across the United States, contributing significantly to the formation of pharmacy deserts. Major chains like Rite Aid, CVS, and Walgreens have collectively closed over 1,500 stores, often in predominantly Black, Latino, and low-income neighborhoods. These closures are partly driven by business competition between independent pharmacies and chains, desire to cut costs by closing underperforming stores, and financial strains from settlements related to the opioid epidemic.
Pharmacy Benefit Managers (PBMs)
PBMs play a large role in the healthcare system by negotiating drug prices and creating pharmacy networks for insurers. However, they often exclude independent pharmacies from these networks, directing patients to specific chain pharmacies instead. This exclusion hits independent pharmacies hard, especially those serving Medicaid and Medicare patients, as they receive lower reimbursement rates compared to private insurers. Furthermore, the lack of price transparency in PBM practices makes it financially difficult for pharmacies, especially in low-income areas, to profit and keep up with operational costs.
Economic and Demographic Challenges
Pharmacy deserts are more common in areas with higher poverty levels, more renters, an ethnic population, and limited transportation options. These areas may also face higher crime rates and lack healthcare professionals, further limiting access to pharmacy services.
Pharmacy deserts disproportionately affect marginalized communities, leading to poorer health outcomes. Residents in these areas face barriers such as longer travel times and medication shortages, resulting in lower adherence to prescribed treatments and this impacts their overall well-being. This situation not only increases healthcare costs, but also worsens health disparities.
Climate Change
The impact of pharmacy deserts is worsened by the increasing frequency of extreme weather due to climate change. These events can disrupt pharmacies and even supply chains, further complicating medication access issues. Additionally, pharmacies often aren’t fully prepared with a protocol to continue operations and deliver care promptly during extreme events. For instance, after a wildfire, patients often need to find alternative pharmacies or providers, adding stress during an already challenging time. As a result, extreme weather conditions only put further strain on a community with limited access to medication services.
Solutions and Takeaway
Several solutions have been proposed and put into action to tackle pharmacy deserts. For instance, mail-order and delivery options have been offered and encouraged to minimize the need for long trips to the pharmacy. There are also mobile pharmacies that bring essential medications, health screenings, and vaccinations directly to underserved communities. With the closure of major chain pharmacies, this also increases the opportunity for independent pharmacies to step in, especially in rural areas, and provide personalized services that cater to the need of the community. However, there is still much that needs to be done, and public advocacy for health equity is needed to properly address this issue. A collaborative effort among local healthcare providers, non-profit organizations, government agencies, and pharmacy associations is crucial to expanding pharmacy services and reducing disparities, especially in marginalized communities. Pharmacy schools should also incorporate education on social determinants of health to prepare future pharmacists for these challenges.
Overall, pharmacy deserts highlight significant healthcare inequities that largely negatively impact the health outcomes of marginalized communities. The complexity of this issue coupled with deeply rooted systemic inequalities makes this a challenging problem to address. It is imperative that we as healthcare professionals stay informed and advocate for change to pave the way for a future where pharmacy services are accessible for everyone.
Winnie Chu
RxPharmacist Team
Resources
- Pharmacy deserts put the health of underserved communities at risk. Available at: https://spotlightonpoverty.org/spotlight-exclusives/pharmacy-deserts-put-the-health-of-undeserved-communities-at-risk/. Accessed August 2, 2024.
- Locations and characteristics of pharmacy deserts in the United States: a geospatial study. Health Affairs Scholar. Available at: https://academic.oup.com/healthaffairsscholar/article/2/4/qxae035/7630415. Accessed August 2, 2024.
- Pharmacy deserts: More than where pharmacies are. PubMed. Available at: https://pubmed.ncbi.nlm.nih.gov/35953379/. Accessed August 2, 2024.
- Access to pharmacies and pharmacy services in New York City, Los Angeles, Chicago, and Houston, 2015-2020. PubMed. Available at: https://pubmed.ncbi.nlm.nih.gov/34366287/. Accessed August 2, 2024.
- Pharmacy deserts and pharmacies’ roles post-extreme weather and climate events in the United States: a scoping review. PubMed. Available at https://pubmed.ncbi.nlm.nih.gov/37431885/#. Accessed August 7, 2024.
Pharmacy Deserts: Navigating the Dry Lands of Medication Access Read More »