Five Varieties of Insulin and Why We Need Them
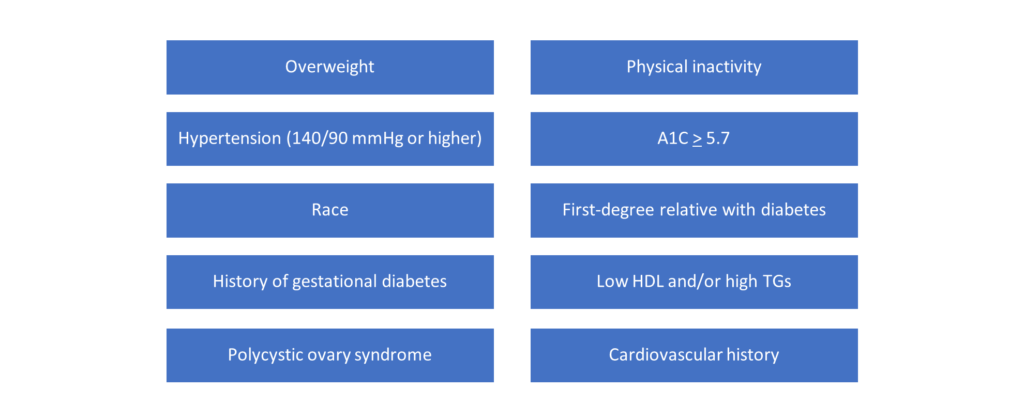
An estimated 34.2 million people in the United States have some form of diabetes (⅕ of which are entirely unaware), and in the last 20 years the number of diagnosed adults has more than doubled in size.1 The significance of this disease state is paramount from a public health perspective, especially as diabetes has been identified as the number one cause of kidney failure, lower limb amputations and microvascular complications.1 You can think of diabetes as a metabolic disease which is generally broken down into four categories: type one diabetes, type two diabetes, gestational diabetes (onset during pregnancy) and prediabetes (elevated blood glucose levels which are yet to be considered entirely diagnostic of active disease).1
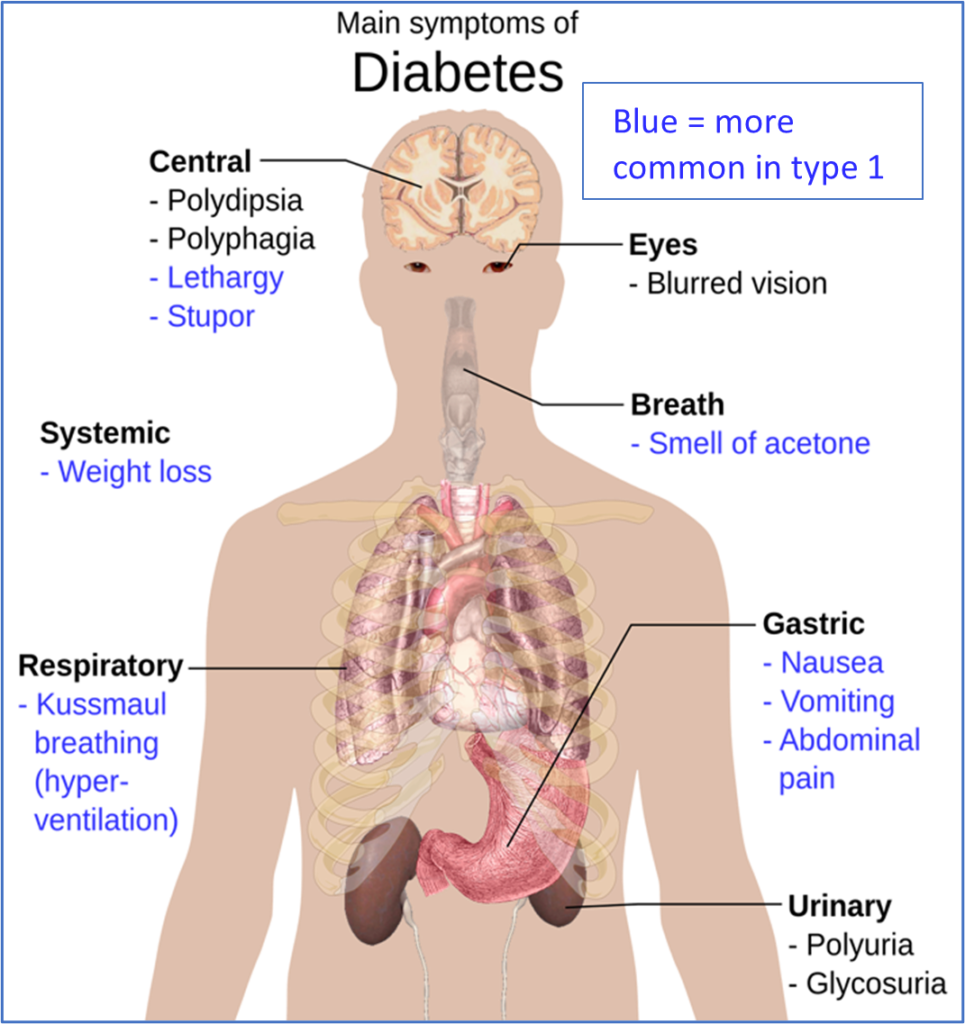
The following video is an excellent visual resource for understanding diabetes and its associated consequences on the human body.6 Both type one and type two diabetes cause an accumulation of glucose in the bloodstream, however, it is the etiology that differentiates them. Type one diabetics essentially experience autoimmune destruction of their pancreatic beta cells which diminishes endogenous insulin production (type one is usually diagnosed in younger people and makes up 5-10% of diabetics).1 In comparison, type two diabetics can produce insulin just fine but their body is unresponsive due to built up insulin resistance over time (type two is usually diagnosed in adults and makes up 90-95% of diabetics).1
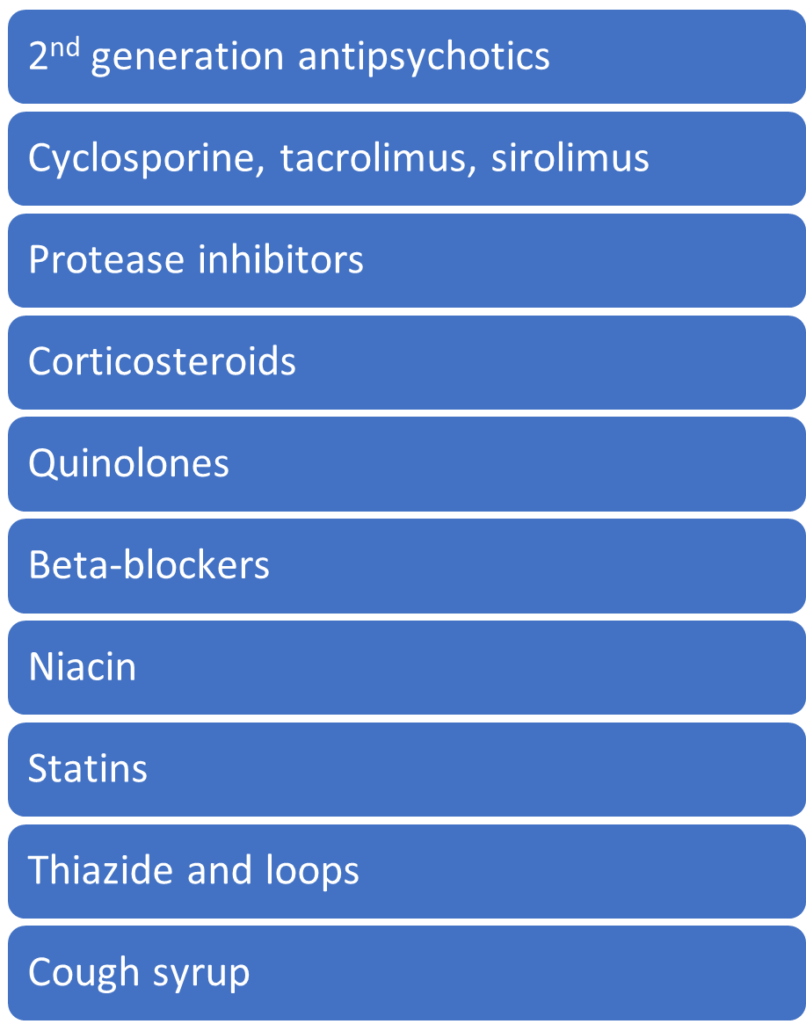
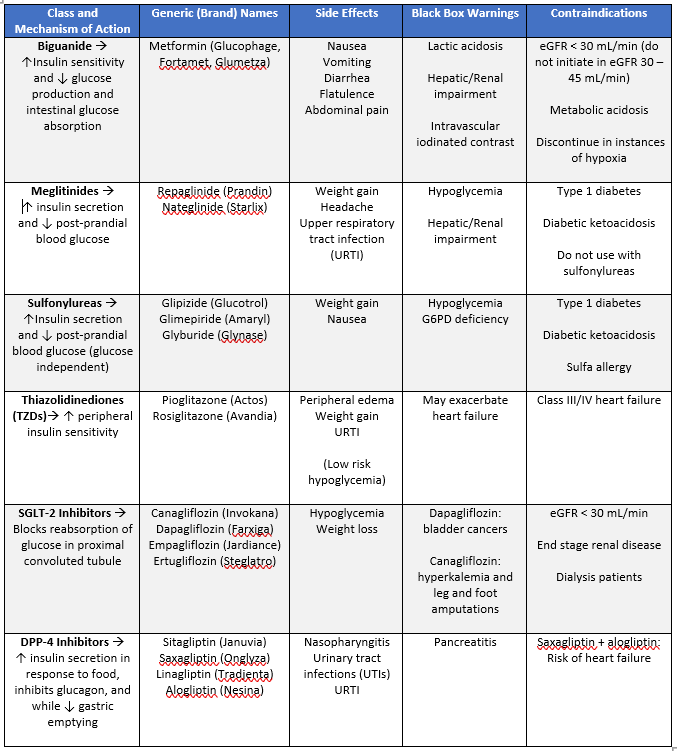
The tricky thing about insulin is it must be injected because it is easily broken down and digested in an oral form.2 All patients with type one diabetes will be dependent on exogenous insulin for survival, and some type two diabetics may also require insulin for adequate control. There is a highly interesting concern in type two diabetes management surrounding a delay in insulin initiation, typically dubbed clinical inertia. You can read more about clinical inertia in the following literature review: Clinical inertia is the enemy of therapeutic success in the management of diabetes and its complications: a narrative literature review.
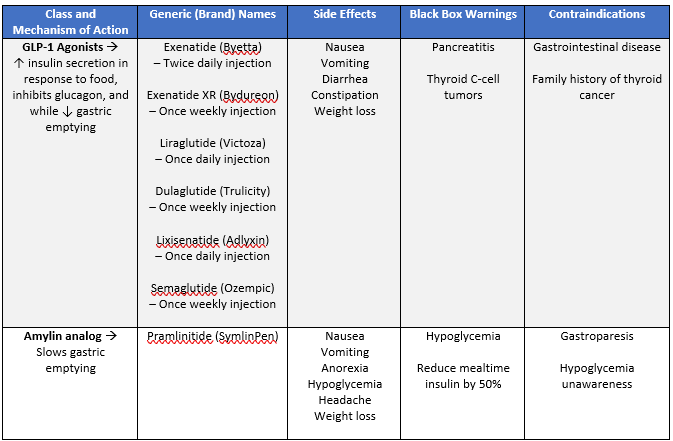
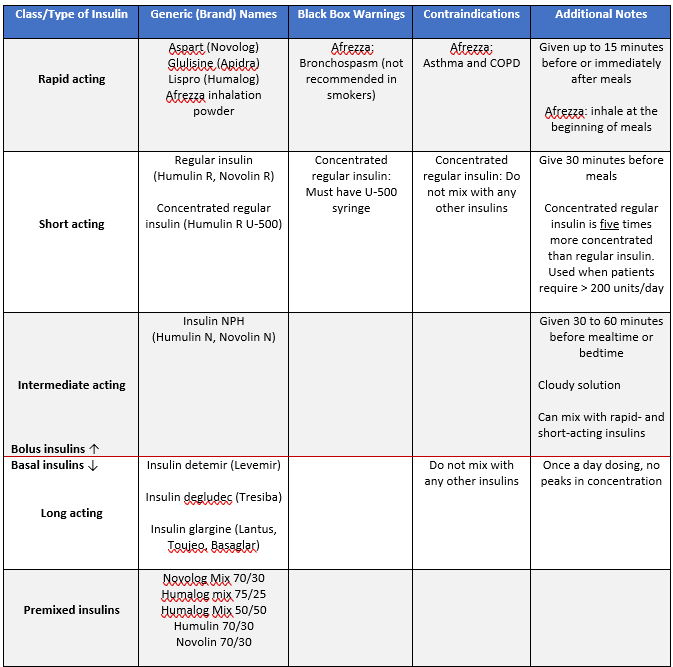
Insulins can be deadly when used inappropriately. It is important to understand and be familiar with the onset, peak and duration of insulins as seen in the figures above so an appropriate personalized regimen or adjustment can be made for each patient’s needs and goals. Generally, rapid and short acting insulins are intended for bolus purposes, whereas intermediate and long acting insulins are intended for basal purposes. We can also categorize and identify insulins via the five categories above. Note that Afrezza is inhaled as opposed to injected and can be given at the start of each meal which may be a great option if a patient is looking for something non-injectable.
As an aside, one important public health issue as it relates to insulins is actually affordability. Supposedly one in four diabetic patients cannot afford their insulin altogether.4 The issue is complex and significant enough to have its own dedicated gofundme page as for many patients insulins are a non-negotiable lifeline. You can read more about the black market dedicated to the insulin trade here, but remember there are resources for patients who need them should you ever directly encounter this issue in the community. Some patients may also obtain over the counter insulin from Walmart’s ReliOn insulin program.
References
- Centers for Disease Control and Prevention. What is Diabetes? Accessed April 6, 2021. https://www.cdc.gov/diabetes/basics/diabetes.html.
- American Diabetes Association. Insulin Basics. Accessed April 6, 2021. https://www.diabetes.org/healthy-living/medication-treatments/insulin-other-injectables/insulin-basics.
- Insulin and diabetes. Accessed April 6, 2021. https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/treating-your-diabetes/insulin.
- About Mealtime Insulin. Accessed April 6, 2021. https://www.humalog.com/fast-acting-mealtime-insulin.
- Teare, K. One in four patients say they’ve skimped on insulin because of high cost. Accessed April 6, 2021. https://news.yale.edu/2018/12/03/one-four-patients-say-theyve-skimped-insulin-because-high-cost.
- Diabetes UK. Diabetes and the body | Diabetes UK. Published September 3, 2013. Accessed April 6, 2021. https://www.youtube.com/watch?v=X9ivR4y03DE.
Five Varieties of Insulin and Why We Need Them Read More »