A Brief Review on Dyslipidemia for Pharmacists
- General information:
- Dyslipidemia is defined as a condition in which an individual has elevated cholesterol or lipids in an individual’s blood such as the following:
- HDL: “Good” cholesterol
- LDL: “Bad” cholesterol
- Triglycerides (TGs)
- LDL cholesterol can form plaques in vessels
- HDL cholesterol helps remove LDL
- TGs are formed in fat cells when calories are not burned right away
- Dyslipidemia is defined as a condition in which an individual has elevated cholesterol or lipids in an individual’s blood such as the following:
- Symptoms:
- Regarded as a silent disease in which patients are unaware of having it
- Types and causes:
- Primary dyslipidemia:
- Inherited through genetics
- Secondary dyslipidemia
- Caused by lifestyle factors such as the following:
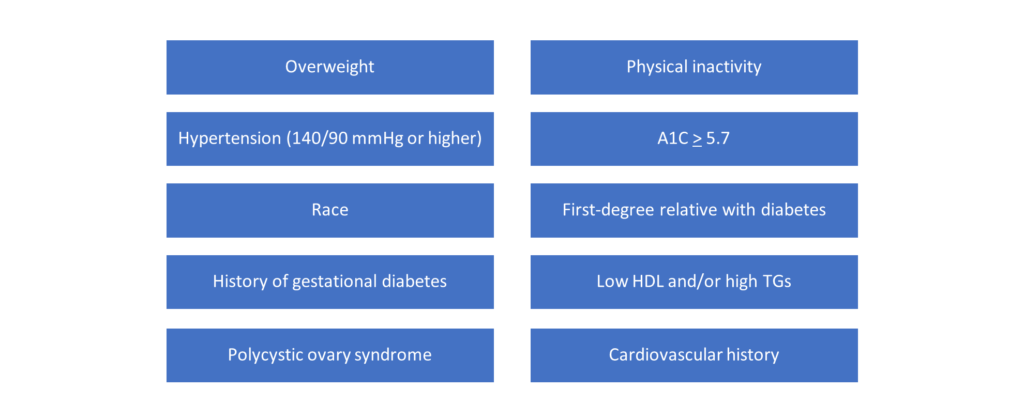
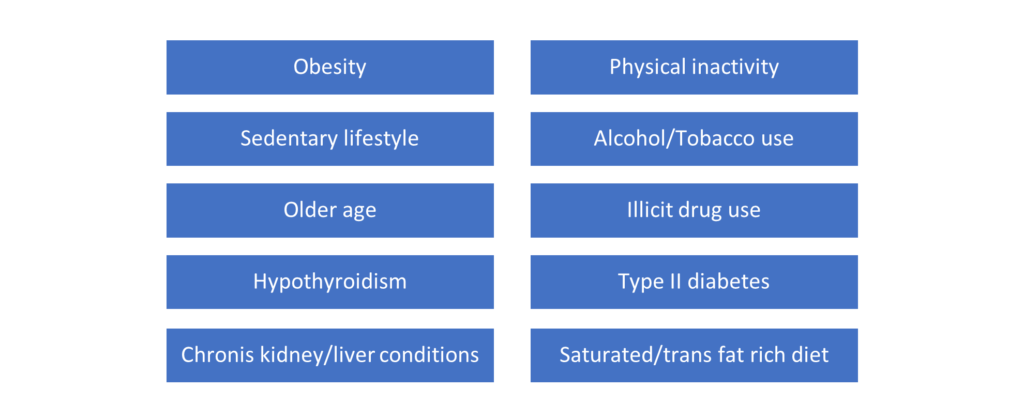
- Obesity
- Diabetes
- Hypothyroidism
- Alcoholism
- Caused by lifestyle factors such as the following:
- Primary dyslipidemia:
- Risk factors:
- Review of lab values**:
| Total cholesterol | HDL | LDL | TGs | |
| Desirable | < 200 | > 40 (men) > 50 (women) | < 100 | < 150 |
| Borderline | 200 – 239 | 130-159 | 150-199 | |
| High | > 240 | 160-189 | 200-499 | |
| Very high | > 190 | > 500 |
**All units are in mg/dL
- Treatment options:
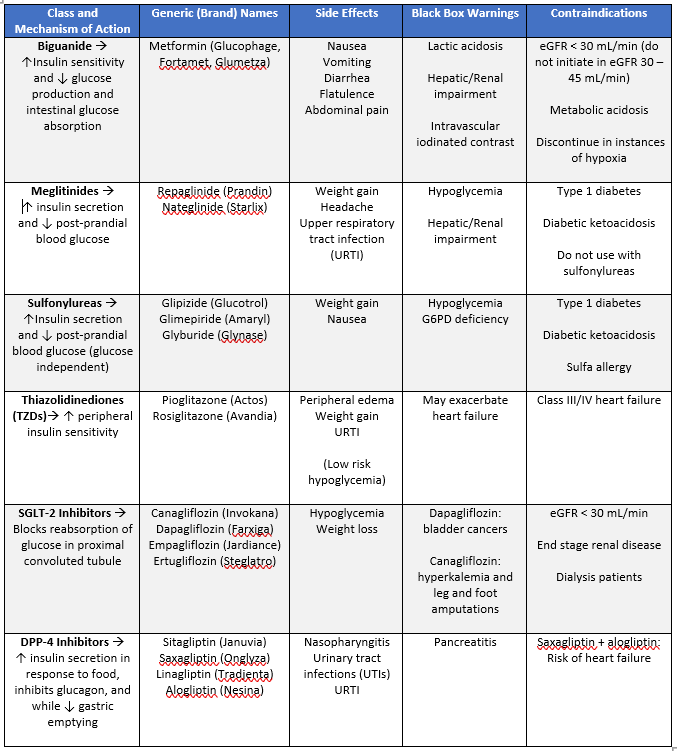
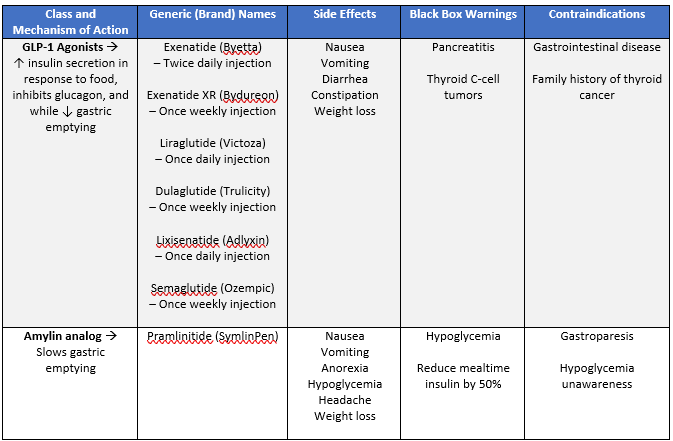
| Class and Mechanism of Action | Generic (Brand) Names | Side Effects | Black Box Warnings | Contraindications |
| Statins: Inhibits the rate-limiting step for cholesterol synthesis by inhibiting HMG-CoA reductase **first-line** | Atorvastatin (Lipitor) Rosuvastatin (Crestor) Simvastatin (Zocor) Pravastatin (Pravachol) Pitavastatin (Livalo) Fluvastatin (Lescol) Lovastatin (Mevacor) Simvastatin + Ezetimibe (Vytorin) | Myalgia Arthralgia Myopathy Diarrhea Cognitive impairment | Skeletal muscle effects Hepatotoxicity (increased LFTs) | Pregnancy Breastfeeding Use with cyclosporine Active liver disease |
| Bile Acid Sequestrants: Inhibits absorption of bile acids into blood which ultimately aids in reducing LDL | Cholestyramine (Questran) Colesvelam (Welchol) Colestipol (Colestid) | Abdominal pain Cramping Flatulence Constipation Increased TGs Increased LFTs Esophageal obstruction | Cholestyramine: Biliary obstruction Colesvelam: Bowel obstruction and TGs > 500 | |
| Fibrates: PPAR-α agonist; inhibits TG synthesis and decreases VLDL | Gemfibrozil (Lopid) Fenofibrate (Tricor) | Abdominal pain Dyspepsia Increased LFTs Upper respiratory tract infection (URTI) | Risk of myopathy with concurrent statin use Increased serum creatinine Cholelithiasis | Liver disease Renal disease Gallbladder disease Use with repaglinide |
| PCSK-9 Inhibitors: Monoclonal antibodies that decrease LDL | Alirocumab (Oraluent) Evolocumab (Repatha) | Flu Cold URTI Injection site reaction Urinary tract infection (UTI) | ||
| 2-Azetidinones: Inhibits absorption of cholesterol at the small intestine | Ezetimibe (Zetia) | Myalgia Arthralgia Diarrhea URTI | Skeletal muscle effects | Avoid in patients with hepatic impairment |
| Fish Oils: Unknown mechanism of action | Omega-3 Acid (Lovaza) Icosapent Ethyl (Vascepa) | Dyspepsia Flatulence Burping Increased LDL | Caution in those with a fish/shellfish allergy | |
| Nicotinic acid/Vitamin B3: Decreases synthesis of VLDL, LDL, and TGs | Niacin (Niacor, Niaspan) | Flushing Pruritis Nausea Vomiting Diarrhea Cough Hyperglycemia Hyperuricemia Orthostatic hypotension | Hepatotoxicity Rhabdomyolysis with concurrent statin use | Liver disease Arterial bleed Peptic ulcer disease |
| High-Intensity Statin Therapy (Lowers LDL on average by > 50%) | Moderate-Intensity Statin Therapy (Lowers LDL on average by 30-49%) |
| Atorvastatin 40-80 mg Rosuvastatin 20-40 mg | Atorvastatin 10-20 mg Rosuvastatin 5-10 mg Simvastatin 20-40 mg Pravastatin 40-80 mg Lovastatin 40 mg Fluvastatin 40 mg Pitavastatin 2-4 mg |
- Additional notes:
- Statins
- Patient must contact their doctor for any muscle symptoms or dark urine
- Simvastatin, lovastatin, and fluvastatin must be taken at bedtime
- Avoid gemfibrozil, niacin (> 1 gram), and colchicine
- Simvastatin and lovastatin:
- Avoid strong CYP3A4 inhibitors such as azoles, erythromycin, clarithromycin, HIV protease inhibitors, cobicistat, nefazodone, cyclosporine, grapefruit juice
- Bile Acid Sequestrants
- Take with food and water (colesevelam)
- Space out with multivitamins
- At least 4 hours of one another
- ACC/AHA guidelines do not recommend use if TGs are > 300
- Fibrates
- Can increase LDL when TGs are high
- Patient must contact their doctor for any muscle symptoms, dark urine, abdominal pain, nausea, or vomiting
- PCSK-9 Inhibitors
- Store in fridge
- Prior to administration allow for syringe to warm up to room temperature for 30-45 minutes
- Inspect for any particles and/or color changes
- Rotate injection sites
- Alirocumab and evolocumab: Subcutaneous injections given in the thigh, upper arm, or abdomen (except within 2 inches from belly button)
- 2-Azetidinones (Zetia):
- Avoid concurrent use with gemfibrozil
- Monitor LFTs with concurrent statin or fibrate use
- Give 2 hours before or 4 hours after bile acid sequestrants
- Patient must contact their doctor for any muscle symptoms or dark urine
- Concurrent use with cyclosporine may increase levels of both drugs
- Nicotinic acid/Vitamin B3
- Must be taken with food
- Monitor LFTs
- Niaspan:
- IR: Flushing/itching
- ER: Less flushing than IR; take at bedtime
- Avoid spicy food and ethanol
- Take 4-6 hours after bile sequestrant acids
- Statins
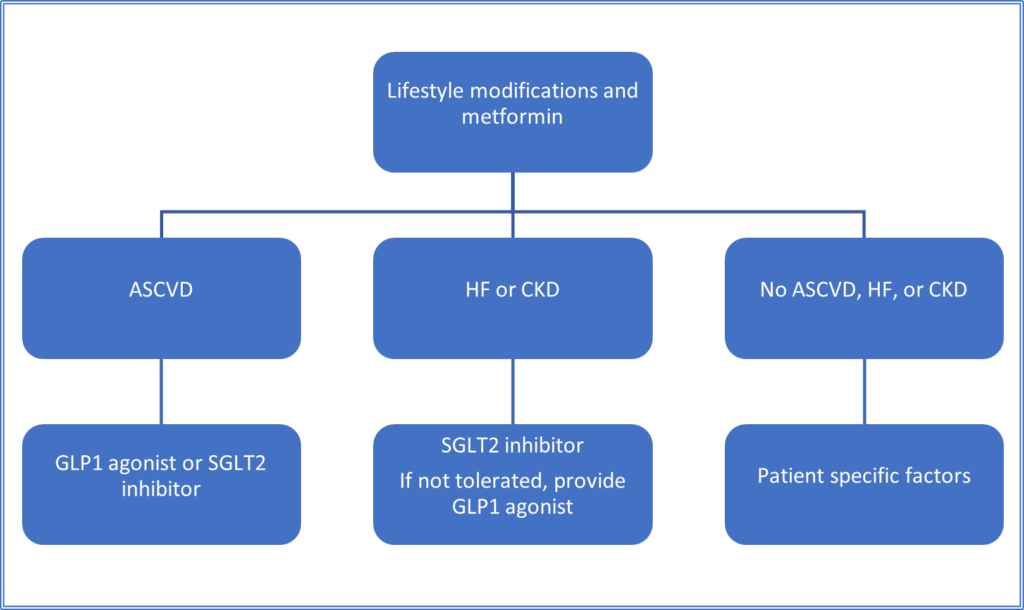
- Treatment algorithm:
| Prevention type | Situation | Treatment |
| Primary prevention | LDL > 190 mg/dL | High-intensity statin |
| Primary prevention | Age 40-75LDL 70-189 mg/dLPatients with diabetes | Moderate-intensity statin, unless 10-year ASCVD risk > 7.5% |
| Primary prevention | Evaluating 10-year clinical atherosclerotic cardiovascular disease (ASCVD) score | ASCVD risk > 7.5%: high intensity statin ASCVD risk > 5% but <7.5%: moderate-intensity statin |
| Secondary prevention | Patients with clinical ASCVD | < 75 years old: high intensity statin > 75 years old: moderate-intensity statin |
We hope this review helped refresh your clinical knowledge on dyslipidemia!
Best of luck,
Sam Tamjidi
RxPharmacist Team
References:
- Micromedex Solutions. Greenwood Village, CO: Truven Health Analytics. http://micromedex.com/. Accessed October 30, 2020.
A Brief Review on Dyslipidemia for Pharmacists Read More »